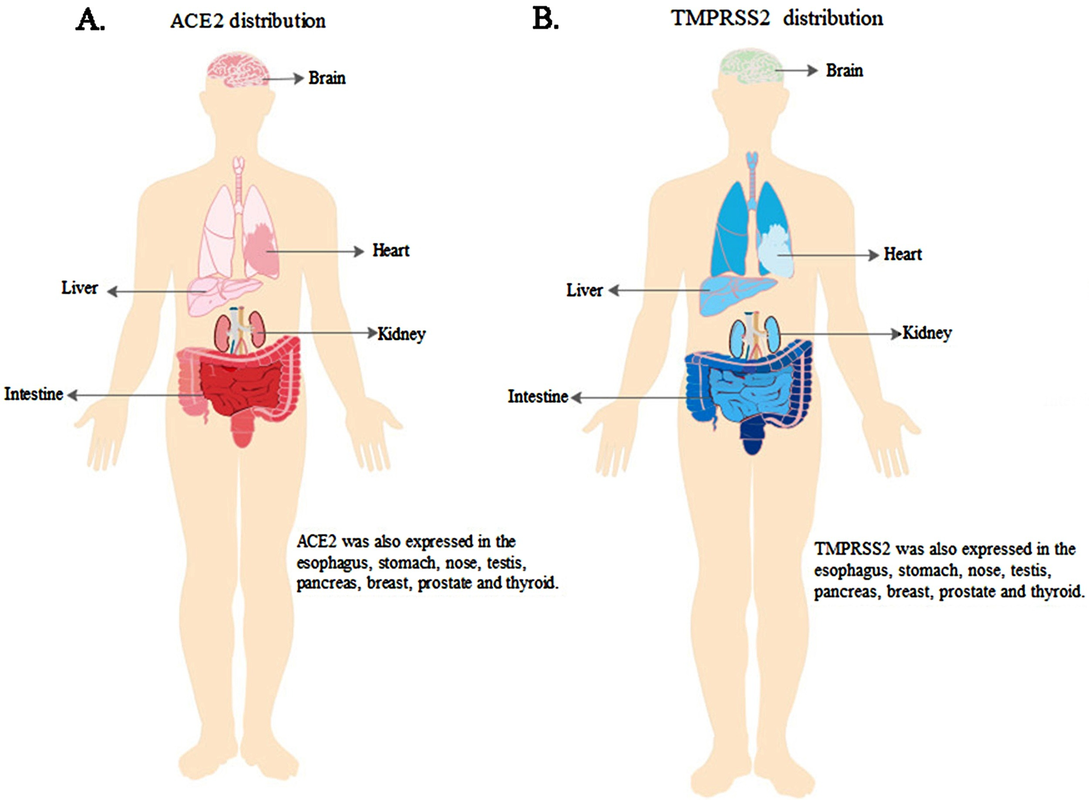
Compiled Rose Rohloff from input by Dr. Peter McCullough and Dr. James ThorpMany persons may have been illegally coerced into taking the Covid shots.(see blog entry regarding the 1974 National Research Act) The following is an extensive Spike Protein (SP-C) lab panel, sectioned into subpanels (a panel is a collection of several lab tests), for evaluating if you systems may have been impacted by the spike proteins - with or without existing symptoms. Note some individual labs may be duplicated in various panels and will not have to be duplicated. Champion your own care and consult with your choice of physician with informed consent. General Tests and Evaluation of Cardiac
The following evaluate antibody (Ab) in your blood, proteins made by the immune system to fight foreign bodies (bacteria, virus …)]**
For women of reproduction age
For autoimmune and/or bleeding issues
1No commercially available test for circulating spike amounts are available at this time and will update as one becomes available. Serum Spike Antibody (Ab) is the surrogate at this time. Higher spike Ab titer correlates with severity of infection/long COVID. Pathologists are able to determine if tissue spike is from Shots/Injections versus infection via correctly performed autopsy, as per Dr. Ryan Cole in deposition of case. “Normal” Value-ranges & Description of various testsSome parameters vary slightly based on which lab is used - low or high readings should be determined by the specific lab being used at the time of lab test, and for individuals regarding their baselines, underlying conditions. D-dimer CBC CRP CMP Various Antibody testing to determine if your immune system is or is not fighting off a foreign substance. TSH: ***
Amenorrhoea Panel
0 Comments
"Ninth Circuit Court Full Details... read each bullet point baby!
(1) The court ruled that the district court misapplied the 1905 Jacobson case because LAUSD relies on a drug that Plaintiffs plausibly alleged did not prevent the spread of the virus. (2) LAUSD has changed its mind about requiring the vaccine and therefore, the case cannot be mooted because LAUSD has proven it will just enact it again later. (3) The court said, "But even if the materials offered by LAUSD are subject to judicial notice, they do not support rejecting Plaintiffs’ allegations. LAUSD only provides a CDC publication that says “COVID-19 vaccines are safe and effective.” But safe and effective for what? LAUSD implies that it is for preventing transmission of COVID-19 but does not adduce judicially noticeable facts that prove this." (4) "Pursuant to more recent Supreme Court authority, compulsory treatment for the health benefit of the person treated—as opposed to compulsory treatment for the health benefit of others— implicates the fundamental right to refuse medical treatment. Plaintiffs’ allegations here are sufficient to invoke that fundamental right. Defendants note that the vaccination mandate was imposed merely as a “condition of employment,” but that does not suffice to justify the district court’s application of rational-basis scrutiny." (5) MUST READ THIS..."In Washington v. Glucksberg, 521 U.S. 702 (1997), the Court explained that Cruzan’s posited “‘right of a competent individual to refuse medical treatment’” was “entirely consistent with this Nation’s history and constitutional traditions,” in light of “the common-law rule that forced medication was a battery, and the long legal tradition protecting the decision to refuse unwanted medical treatment.” Id. at 724–25 (citation omitted). Given these statements in Glucksberg, the right described there satisfies the history-based standards that the Court applies for recognizing “fundamental rights that are not mentioned anywhere in the Constitution.” Dobbs v. Jackson Women’s Health Org., 597 U.S. 215, 237–38 (2022). The Supreme Court’s caselaw thus clarifies that compulsory treatment for the health benefit of the person treated—as opposed to compulsory treatment for the health benefit of others— implicates the fundamental right to refuse medical treatment." https://cdn.ca9.uscourts.gov/datastore/opinions/2024/06/07/22-55908.pdf… by Rose RohloffTHE ORIGINAL HIPPOCRATIC OATH ALTERED & EXPANDEDCaring for health will not improve until we bring back oaths: binding testimonials for committed healers. The privilege and honor of being in charge of lives with integrated souls is not a job; it is a calling. We, individual Christians - not schools, governmental agencies or regulatory bodies - hold each other to the highest standards. And, oaths are taken and upheld by individuals. The following expansion on the original Hippocratic oath is for MD/DO/DC, PA, RN/LPN, Naturopath, Therapists, etc. anyone within the industry of healing. I (name) will perform my duties with faith and trust in God as my guide, and continually learn as long as I perform my duties. I will impart a knowledge of the art of healing, mentoring and teaching those I serve. Above all else, I will abstain from whatever is deleterious, mischievous, malfeasance or unjust to those being treated, and I will not break what is not broken, for that is doing harm. Clinicians post degrees; what about posting the oath
they abide by, adhere to, and practice within its ethos? Who is in charge of healthcare? Is your Health insurance coverage invalidated/exempt? 5G and edc4/12/2024 by Rose RohloffEach individual should be in charge of their own healthcare decisions, safety surroundings, and be treated individually. So, a good question to ask, "Who actually is in charge?" Laws and Executive Orders (EOs) regarding healthcare under "public health"Created by Todd Calendar, Esquire H.R.3832 - Disease X Act of 2023 118th Congress (2023-2024) Open "disease" cart blanc for them to choose (or orchestrate?) ‘World Health Organization (WHO) Has No Authority to Dictate U.S. Health Policy’ factcheck.org March 2, 2023 "Although the accord is being called ... a treaty or another kind of binding agreement, such as the WHO Framework Convention on Tobacco Control, or a nonbinding agreement, such as the Paris Climate Accord. “As with all international instruments, any accord, if and when agreed, would be determined by governments themselves, who would take any action while considering their own national laws and regulations,” a WHO spokesperson told us." Federal and Local Governments would be in charge regarding any Rights violations. The accord is accumulation of monies $$$ to be "distributed" to various countries/persons, in the name of public health.
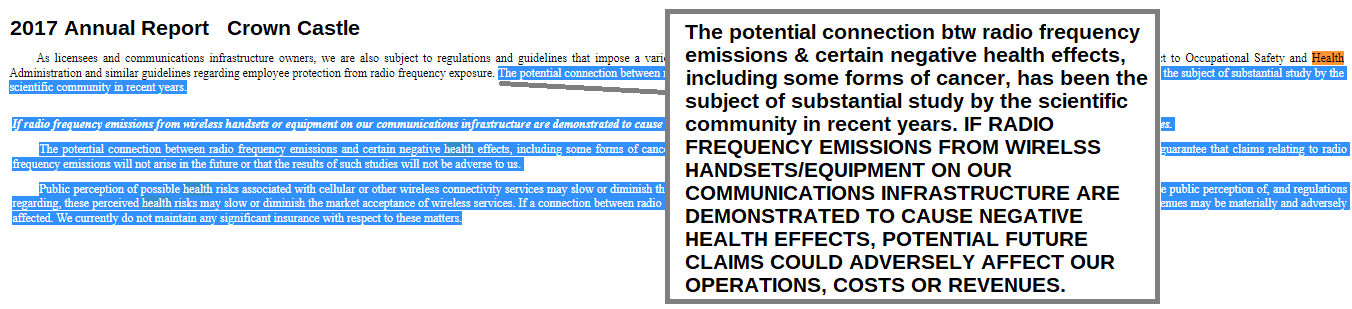
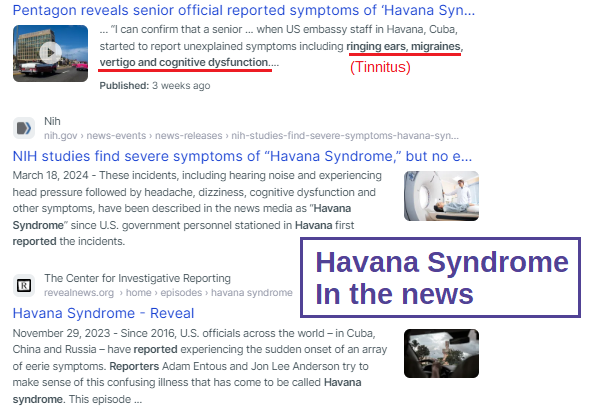
LTC (ret) Green Beret, Doc Pete Chambers, MD, bioweapons expertRisk of 5G rolled out, without safety studies, by Federal, State and Local governance. Communities were not asked regarding rollout, or informed regarding safety issues of 5G. Are we experiencing history repeating the dangers of DDT, Asbestos, many FDA "approved" drugs recalled because they lacked safety, etc.?
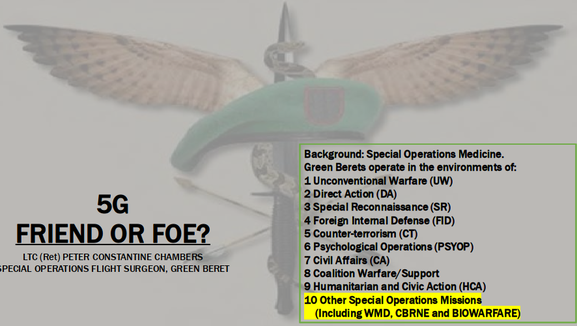
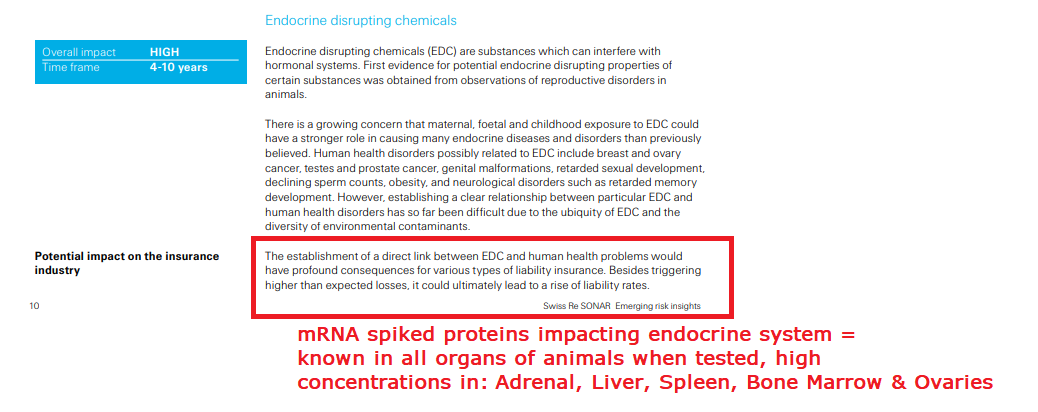
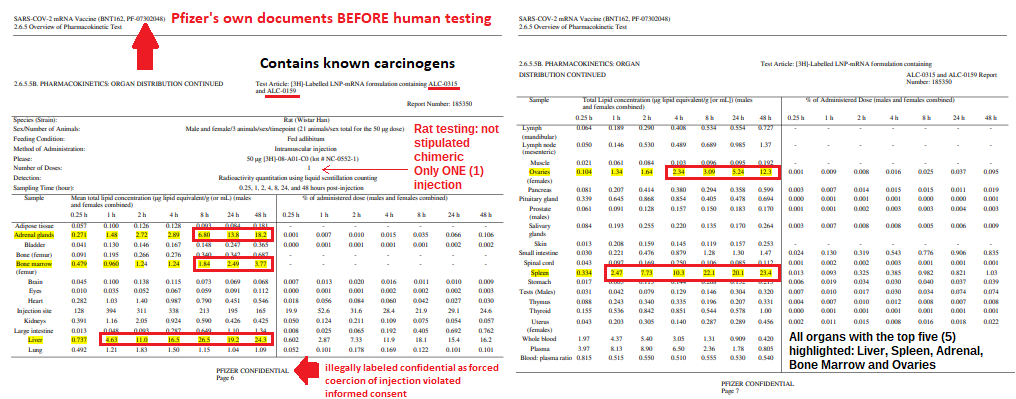
Are individual healthcare insurance policies, the underwriters of policies, being invalidated without the knowledge of people, and against their choice - through lack of knowledge, lack of informed consent, and through illegal coercion? Electromagnetic RadiationEndocrine Disrupting Chemicals (EDCs)by Numerous expertsMy desire is to provide several articles from those adroit in the subject. COPPER: the less talked about, and important trace mineral, the importance of Zinc, and when taking high Zinc, make sure you know the ratio of zinc to copper supplements.
Ralph Baric and other scientists knew in 2010 the "antidote"/treatments for the upcoming virus(es). He coauthored the discovery "Increasing the intracellular Zn(2+) concentration with zinc-ionophores like pyrithione (PT) can efficiently impair the replication of a variety of RNA viruses". Dr. Vladimir Zelenko based his effective protocol after watching the "MedCram Lecture 34 by Dr. Roger Seheult about the use of zinc and zinc ionophores. Zinc is an essential mineral for humans, and a little extra zinc is sometimes used to lessen the intensity of colds and sore throats. An ionophore is a chemical that opens the cell wall to allow minerals (ions) to enter. ‘First do no harm’ Zinc is an over-the-counter supplement. Hydroxychloroquine (HCQ) is a reliable ionophore, and it has a well-established dosing regimen and safety profile." Zinc ionophores "increase the intracellular concentration of Zinc ions causing significant biological effects. Review ionophores: HCQ, EGCG (a plant compound particularly prominent in green tea) and Quercetin (particularly in citrus fruits, apples, onions, parsley, sage, tea, and red wine. Olive oil, grapes, dark cherries, and dark berries such as blueberries, blackberries, and bilberries are also high in quercetin and other flavonoids.) "
Mount Sinai "Copper is a mineral that is found throughout the body. It helps your body make red blood cells and keeps nerve cells and your immune system healthy. It also helps form collagen, a key part of bones and connective tissue. Copper may also act as an antioxidant, reducing free radicals that can damage cells and DNA. Copper helps the body absorb iron. Your body also needs copper to make energy."
Dr. Shiva The Power of Copper to fight virus, bacteria on contact
Copper has even been shown to be very effective at exterminating the much-dreaded hospital ‘superbug’ MRSA. In tests sponsored by the Copper Development Association, a grouping of 100 million MSRA bacteria atrophied and died in a just 90 minutes, when placed on a copper surface at room temperature. The same study found that the same number of MSRA bacteria on both steel and aluminium surfaces actually increased over time. On looking at these figures, many scientists have concluded that the installation of copper-based fixtures such as taps, light switches, door handles, door knobs, pull handles, and push plates in areas such as hospitals could save thousands of lives each year.
Professor Bill Keevil, head of the microbiology group at Southampton University, added his voice to the growing scientific consensus behind this by advocating the use of Copper and Brass door furniture, fixtures and fittings in public places and on public transport, as they could dramatically cut the threat posed by superbugs. In research published in the journal Molecular Genetics of Bacteria Professor Keevil wrote: “There are a lot of bugs on our hands that we are spreading around by touching surfaces. In a public building or mass transport, surfaces cannot be cleaned for long periods of time… Until relatively recently brass was a relatively commonly used surface. On stainless steel surfaces these bacteria can survive for weeks, but on copper surfaces they die within minutes… We live in this new world of stainless steel and plastic, but perhaps we should go back to using brass more instead.” In addition to direct contact killing of bacteria and harmful microbes, amazingly Copper surfaces have been found to exude an antimicrobial 'halo' effect on surrounding non-copper surfaces. Research in the intensive care unit a Hospital in Greece found that other surfaces up to 50 centimetres from copper surfaces experienced 70% microbial reduction, compared to the same surfaces with no proximity to copper-based materials. The ‘Halo’ effect was also observed in trials at a U.S. clinic in 2010. This amazing effect demonstrates just how powerful copper is as a weapon against bacteria." www.morehandles.co.uk by Rose Rohloff
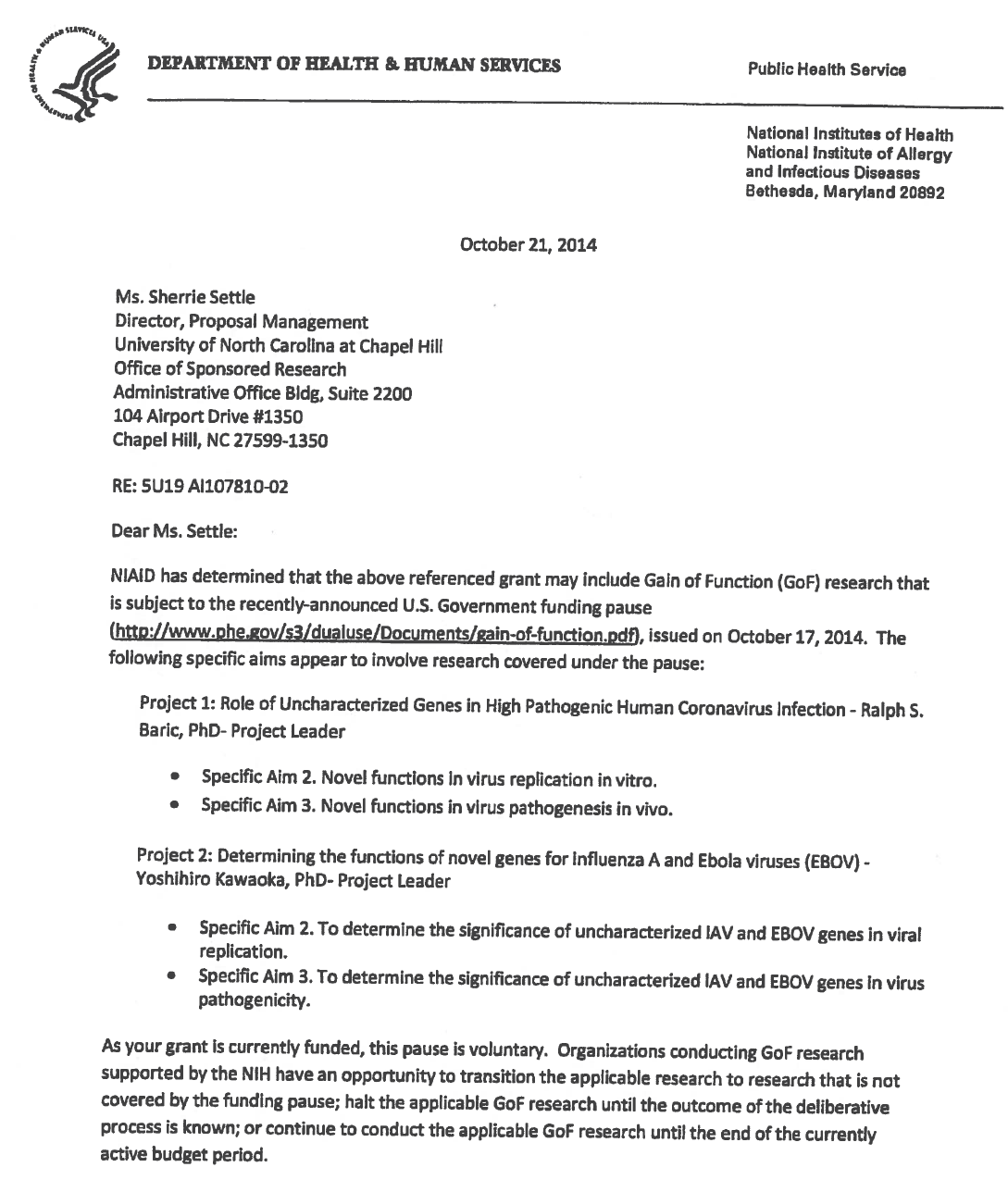
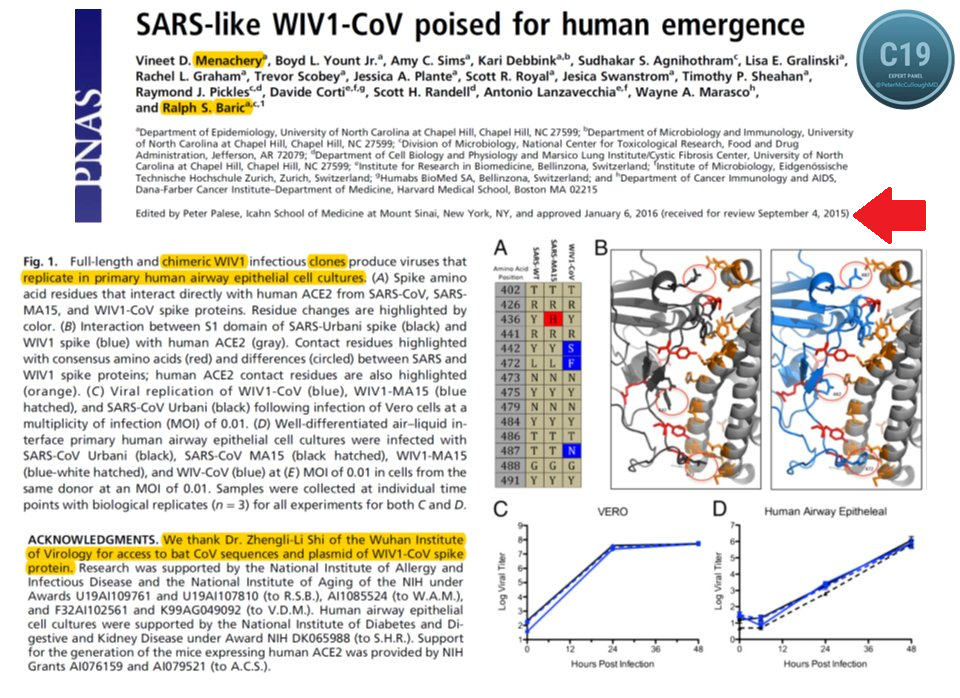
* Date: written 2015 posted 2016
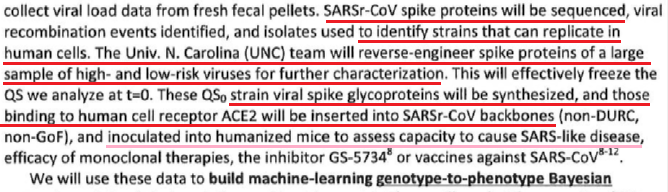
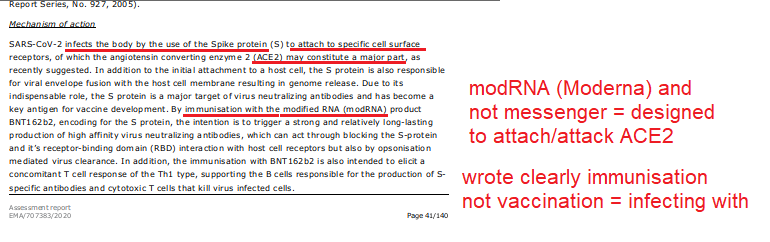
* Not natural: chimeric infectious clones, GOF Listen with this link https://thehighwire.com/ark-videos/aaron-siri-gives-testimony-on-the-floor-of-arizona-state-senate/ FDA working in support of pharma - no clinical trial testing of vaccines with "circular approval."
by Rose Rohloff An India folklore, regarding lack of awareness, demonstrates the current myopic view of various specialists, who look at isolated symptoms without comprehensive assessments, resulting in poor or lack of diagnosing of real issues to address in patients. The industry push to eliminate primary care, teaching people they don’t need a primary doctor, or using primary care doctors as simple pass-through without diagnosing, handing off to multiple other doctors, has resulted in the loss of care coordination, overdosing multiple medications with contraindications/side effects, with increased conditions because multiple doctors only look at their individual view. The following version of the blind men and the elephant story is from Peacecorp.gov, and is analogous to the existing healthcare system of specialists. Long ago, old blind men were curious about the many stories they heard about elephants. The men were led to one for each person to independently touch the animal.
All body systems impact each other, designed to function as a whole, for a well orchestrated, compensatory mechanism. By only looking at individual symptoms of isolated systems, patient’s underlying conditions are not addressed for health, and can often be fulminated and/or obscured by medications. And, the reason primary care doctors are imperative for knowing the whole patient, knowing how to diagnose and treat many conditions. Primary doctors should only pass their patients to specialists for complicated, complex conditions, while always following their patient and maintaining all coordination with any other doctors.
With perpetual reporting of the COVID-19 virus, there has been a lot of panic reaction from the public, fostered by the media, as well as from local clinical staff. These reactions have brought existing issues in the healthcare system to the forefront, that we can address go forward, especially for discernment to champion better quality of care. The following two use case examples happened last week, which demonstrate panic reactions from clinicians, the need for good primary care, and the need to address care standards, especially in crisis, with sense at the delivery level. An immune suppressed mother has three children, one being a 10 yr. old daughter who woke with a 102 temperature and a sore throat. The mother is not reactionary, having good instinct regarding when her children are fighting off bugs, building up their immune systems. She phoned the pediatrician to ask for testing if it is strep or a virus. The pediatrician stated they only test for COVID-19 if someone is hospitalized, and they would not do a strep test, “Don’t bring your child in”, and then the pediatrician went on a rant about social distancing, “This virus will not end …” (with no reported cases in the area) etc. and simply ordered Amoxicillin. I don't want to give my daughter an antibiotic if she doesn't need it, and especially if it is a virus, let alone the Corona virus." Removing all emotion from the situation with her, we discussed getting zinc in EZC Pak from the CVS a mile away, that she could pick up via their drive through, along with foods high in Vitamin A to boost her daughter's immune system. I also called the local Urgent Care center explaining the situation: a mother immunosuppressed, her daughter is in the EMR system, she just wants a strep swab to avoid unnecessary antibiotics, to please have a nurse do the swab through the car window when she drives up - avoiding any cross contamination issues. They stated no problem.
The same week, a second mother of four small children, one being a seven year old who was having sore joints and some blood in her urine. The doctors in Green Bay did a wonderful job of a full, very detailed history and then exam with targeted tests, quickly diagnosing Rheumatic Fever. Her and her other three, healthy children were instructed to do proactive strep testing since they all had close exposure with the daughter. "The center made us feel like lepers. Instead of simply coming out to the car to meet us, they brought us to an empty lobby with a nurse who came out in a full hazmat suit to do simple strep swabs. The nurse freaked out when my son simply cleared is throat, creating anxiety, complaining, "He just coughed." The clinicians throughout both cases should have been calming, simply asking good questions, and then only ordering the correct test before ordering medication. And, in both cases, clinicians could have had the tests quickly, avoiding the waste of hazmat gear, not frightening healthy family members as well as not exposing them to potential germs in the health facilities - avoiding cross contamination issues. What we need to focus heavily on:
One point stood out regarding their focus that is so often missing in health systems: seeing 'clean' patients first, and then seeing contagious patients grouped together, ensuring avoidance of cross contamination, and minimizing the volume of masks, gowns or hazmat suits used.
Hopefully, many good things will come from this virus experience to positively shake up our healthcare system, including basic sense procedures, with the importance to rebuild and focus on great primary care again. Another glaring issue to address is the role of clinicians as cool, calm professionals, removing emotion when instructing with full information, with clearly explained options for informed consent and decision-making for delivery of quality care. by Rose Rohloff It is known taking medications will impact various lab values. For example, Diuretics e.g. Lasix (Furosemide), can cause low potassium levels. There is an interesting article in Medscape, Which Drugs Interact With Lab Tests? Jun 18, 2019., addressing the fact that certain medications can also interact with the actual processing of certain lab tests causing inaccurate results.
by Linda LybertPresident/ Healthcare Surfaces Expert, Founder/Executive Director Healthcare Surfaces Institute Privacy curtains must be addressed and as I talk with healthcare professionals about this issue I get mixed reactions. Digging deep into the issue the biggest problem is the amount of time and labor it takes to actually change the curtains out. "It is backbreaking and we don't have enough staff to actually do this on a regular basis." Every facility sets its own standards for changing privacy curtains and the responsibility lays with operations. Policies range from change when visibly soiled (NOTE: microbes can't be seen) to once a quarter and even once a year and any time in-between. As research continues to be published it is clear to mitigate the spread of infections solutions this must be part of a solutions bundle addressing all surfaces! See LinkedIn Post with full Study: Patient Privacy Curtains represent Infection Risk Linda Lybert is an amazing expert in healthcare surfaces. The same circumstances existed 20 yrs ago, but clinicians were properly trained & executed safety processes/avoided cross contamination; learning in school movement memory e.g. wash hands after closing curtains before touching patients, use elbows to open curtains to enter or push all the way open, etc. #1 issue - lack of clinical training, laziness, and inadequate adherence of movement memory for proper safety protocols. Rose Rohloff
by Rose Rohloff The 2009 HITECH Act and the Center for Medicare Medicaid Services’ (CMS) Meaningful Use regulations caused a massive spend for electronic medical records (EMRs), the push for interoperability, as the solution to healthcare quality. However, EMRs are not solutions - along with massive IT overhead spend with decreasing quality - because in a high percent of instances, nurses and doctors don’t even read them. A 40-year old mother went to the doctor after treating herself holistically for some laryngitis, stuffy nose, congested sinus, with continued symptoms after five days. After an exam, the doctor stated, “I am not going to give you antibiotics. You do not have a fever; your lungs sound clear. It looks like a little virus with severe allergies. I recommend an antihistamine.” The patient told him, “Thank you for not putting me on antibiotics when they are not needed, that makes me happy.” He responded, “I am glad you are glad.” He then said something and the patient responded, “I have MS.” He responded, “Oh wait, you have Multiple Sclerosis?”
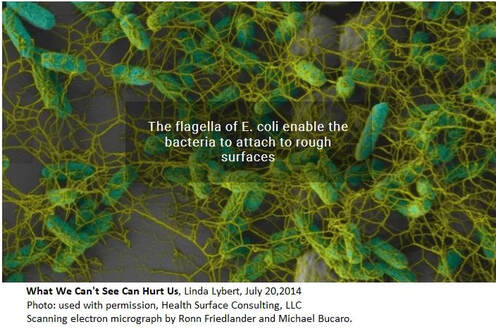
This story is sadly too often the new normal, numerous instances of patients and their caregivers stating issues of diagnosing with medication prescription, or misdiagnosis; the doctor or nurse having no idea of pre-existing conditions or a full list of medications currently being taken, a lack of care coordination or care planning because the time was not taken to simply read the chart (whether written or electronic), and ensuring a comprehensive history followed by the necessary physical assessment. No physician or nurse should walk in to care for a patient without first having read the patient’s record, knowing all current information, the last visit/healthcare encounter, chronic conditions/comorbidities, and all medications; then, asking for updates of changes. Unfortunately, even without having to decipher poor handwriting, being able to read clean typed text, clinicians are not simply reading the basics of information they should before doing any diagnosis, planning and care, or prescribing of medications. by Rose Rohloff The baby boomer generation is now the growing population of elderly with more care needs in home health. As the current generation is being faced with the care responsibilities, many are still unaware concerning various facets of caring for others: advanced directives and living wills; stimulation and diets for mental sharpness, questions to ask and quality of care considerations with becoming power of attorneys - the core of healthcare awareness. One area is focused heavily within hospitals and other care delivery environments, but yet over looked in private homes – surface areas and cleanliness. A popular trend in houses is the use of marble and granite as counter tops. A leading surface expert, Linda Lybert President of Healthcare Surface Consulting stated, “Granite and Marble are like large sponges you cannot wring out.” The photo displayed shows the build up of E. coli bacteria in the pores of stone. According to Ms. Lybert, even when sealed, the porousness is reduced, but not eliminated. And, bleach is not able to eliminate once they reside in the crevices. All surfaces in the home, counter tops, floors including laminates, tile and grout need diligent daily cleaning and disinfection. However, Ms. Lybert brings awareness that regarding "stone surfaces, including granite/marble, there is no effective means to disinfect these surfaces." Consider, "granite is an underground aquifer for our water filtering out all kinds of things. Given the right kind of environment, heat and moisture, bacteria will grow."
As the elderly begin to lose their mobility and agility, it is important to maintain clean surfaces in bathrooms and bedrooms, along with the most important surface being the skin. Diligent hand washing and bathing is important throughout the day to avoid cross contamination from the loved one you are caring for, as well as to them. The other surface area to be conscientious of is bedding. When excrement accidents occur, it is important to wash bedding with very hot water to not only clean them, but also kill the microbes. Clostridium difficile (commonly known as C-diff) "is in the community and found in outpatient settings. There are significant risk factors in patients who are immunosuppressant, individuals who have been on antibiotic therapy, and the elderly population." C-diff is a secondary, very dangerous and potentially deadly infection after antibiotic use. [read article] It is important to those in the community to have appropriate antibiotic prescriptions and use, especially avoiding unnecessary broad spectrum antibiotic use which targets the "good" bacteria you need internally (and not on external surfaces) to kill off C-diff. by Rose Rohloff |
||||||||||||||||||||||||||||||||||||||||||||||||||
| Value is a relative term based upon personal perception, and oftentimes great marketing. True value is based upon insightful knowledge of what entails quality along with the cost of delivering goods and services. Value-based care is the new buzz for basing reimbursement in the healthcare industry. But again, what is value care: personal perception, marketing, cost? |
The primary issue with such score deviations is determining if poor marks are isolated instances (one offs); or, if the variance of only highest and lowest reflect the knowledge of reviewers. Are the high ratings from non-healthcare persons based on perception of the veneer friendliness and scheduling, with one star comments based on specific quality requirements, care competency posted by those with healthcare insight/experience?
As a 35+ year healthcare veteran, an answer was determined accompanying a Medicare patient ‘John’, in his mid-80s who experiences early stage dementia, to the office for a post-op visit for a leg stint placement.
| Upon arriving, another elderly patient (80s) was sitting outside, unattended in wheelchair, hot sun, 100 degree weather, no water. When asked why he was there, he stated, “I can’t stand the freezing air conditioning inside while waiting for a ride.” After walking John into the lobby, the gentlemen clearly seen through the glass door was pointed out to the receptionist stating that he was left in hot sun, no water, unattended. The receptionist stated, “It is his choice to stay out there.” I then stated, “Get someone to check on him, give him water, put him in the shade and check when his ride is supposed to arrive and monitor him if it is delayed or bring him inside.” One person escorted us back to exam room. She did not introduce herself or her title. She proceeded to take the blood pressure with no other vital signs (unknown if a secretary, an aide, a nurse or tech). She then asked the patient, “How much do you weigh?” He gave a number. As patient champion I responded, “He doesn’t know, he has not weighed himself. You need to weigh him yourself.” She responded, “We don’t have a scale.” She then left. I followed her witnessing her documenting the incorrect data. | I reiterated he has dementia with no idea how much he weighs. She replied, “It doesn’t matter anyways, we just need to put something in the record.” She was reflecting an 11 pound weight loss from previous recording. It is unclear if they performed the previous weighing, if it was done just prior to surgery to determine proper anesthesia delivery for his surgery. Another woman in scrubs entered the exam room without introducing herself or her title, asking John to remove his shoes and socks. (The scheduled appointment was with the PA so the patient assumed her identity.) She asked him if his wound was healed and he replied, “Yes.” She documented something in the chart without ever assessing his wound for healing or determining if there was infection. She bent down and felt his feet with her whole hands stating they feel warm, and then asked if he had numbness in his feet. John responded, “Yes.” | Having worked as a registered nurse (RN) in cardiovascular and neuro intensive care units (ICUs), I know she never did pedal (foot) pulse checks x4 comparing both feet. She never assessed location of numbness, or if chronic/intermittent, positional with sitting/, standing, walking, etc. The family had asked if aspirin could be stopped as the patient has experienced nose bleeds in the past. The staff person responded yes and since there was 90% blockage of the previous stint, it was cleaned out and continue Plavix. There was no establishment of lab work as part of care plan determining effectiveness of the medications, especially since the previous stint occluded. "1,750 or so stent patients are also prescribed Plavix to prevent clots from forming around the stent, but of that group, approximately 500 (29%) carry a genetic variation that prevents them from converting Plavix into its active form. This gene-related lack of response stands to be "especially severe" in about 50 (3%) of those patients, who won't derive any benefit from Plavix - 2010 Vanderbilt Medical Center |
Perceived value based on quality versus true value and cost
The care competency and quality as true value-based care during the visit includes:
- lack of basic cleanliness standards with severe cross contamination practices
- no introduction of name or title of any staff member
- fraudulent documentation in the electronic medical record (EMR)
- no assessment performed during a specific post operative visit (a family member could have taken the BP and said his feet felt warm.)
- lack of care planning and evaluation of medication regime
- unnecessary secondary office visit charging for follow up
- another elderly patient left unattended in the hot sun
If the U.S. healthcare system wants to achieve true value-based care, we need an educated population, higher accountability of staff standards with the ability to send evaluations direct to payers based on specific facts and not emotion, and surveys must include care competency reviews versus only veneer questions of politeness, room appearances, and on time scheduling.
| As the dark side of IVF slowly comes into focus, even more transparency is needed by Pamela Mahoney Tsigdinos, July 27, 2018 |
The June 29, 2018 BECKER'S Hospital Review article shares the viewpoint "Froedtert CEO Cathy Jacobson: Not every patient needs a primary care physician" (PCP). The article is the perspective from the viewpoint of a health system CEO. The following is a perspective, counterview from patients, the individuals in the population.
Many people have expressed utter frustration from lack of a good Primary Care Doctor, warranting unnecessary ER visits because a doctor will not call back; the lack of one doctor in charge who would simply LISTEN to them, who knows them - not as personal friends, but with an in-depth professional relationship.
I have been asked several times in various states, "Do you know of any good Primary Care Doctors? I cannot find one." Universally, I am hearing: a gross lack of comprehensive assessments from doctors; clinicians not taking the time to get to know and listen to what is going on, causing the passing through of patients to specialists versus a primary care doctor creating a plan of care and focused tests for getting an actual diagnosis; lack of avoidance for hospital visits with increasing costs that could and should be avoided because conditions allowed to worsen; and doctors simply writing prescriptions for symptoms.
Her quote continues, "... insight further into consumer driven wants, we are finding that a substantial sector of the population does not want or need a primary care physician relationship. People need primary care but not necessarily a physician relationship." The issue is the primary care physician practices have been acquired by the hospital-health systems, with the biggest complaint from people in the population not being able to find a PCP; and those now under health systems, the doctor only giving 10-15 minutes of time, before passing off to specialists with no plan of care, and/or simply writing another prescription. Many in the public just find it faster, or are being told to just go to the ER. From the perspective of health system CEOs, it would appear primary care is not wanted or needed, which drives up the hospital ER and inpatient business. When actually speaking with individuals across the country, it is the opposite, people complain lack of care coordination, and "the doctor doesn't know me and is not taking the time to listen to me - I want them to actually figure out a diagnosis of what is wrong."
Kyle Reyes, CEO, The Silent Partner Marketing
The solution is bringing analysis down to the most base level of management with front line analysis, to coincide with first-hand observation, the voice of the patient & their caregivers/champions, and reducing the ever growing administrative overhead. Bigger is not better for addressing health and care of populations, when the focus is shifted upward with large systems where individuals are lost: Especially when the individual issues are indicative of the core problems that need to be addressed for quality care delivery.
The need for P&P Reviews
| by Rose Rohloff | HealthLeaders published an article Proper Sharps Management in Senior Living Helps Reduce Risk for Needle Stick Injuries Feb. 9, 2018, addressing the need for proper containers to safely dispose of used needles. Sadly, stories have been relayed regarding used syringes being left in the beds of patients in hospitals and rehabilitation facilities. As trained clinicians, this circumstance should never happen. The issue of needle-syringe safety, however, transcends all environments, including the increasing use in homes. Safety guidelines for syringe use |
- Have designated, well marked containers for immediate disposal (reference the Healthleaders article above)
- Use the one touch rule: after injecting medication, do not set the needle down; immediately drop into the designated, marked container.
- Do not recap the needle unless necessary. To avoid sticking oneself, drop the syringe directly into the container without recapping after used. If the needle requires coverage for immediate safety, keep the cap on a flat surface (such as a table) while inserting the needle. Then, lift the syringe with the cap on to firmly secure it against the table; avoiding needles accidentally being pushed through a cap, or missing the cap opening and puncturing your finger.
- Properly dispose of needle containers. See CDC recommended guidelines.
| by Rose Rohloff | Another common practice over the past decade is the prescription of broad spectrum antibiotics for non-life threatening conditions. Broad spectrum antibiotics are for use in life threatening conditions/sepsis when there is no time to wait for a culture, or the inability to do a culture. Broad spectrum antibiotics target the necessary bacteria needed in the adult intestinal tracts; and so, the standard practice has become the second prescribing for probiotics; the requiring of multiple medications to be taken. Additionally, numerous reports over the last 10 years have shown the continued misuse of antibiotics (e.g. CDC Grand Rounds) causing antibiotic resistance, with the need for more and more antibiotics to be created and used. |
What has caused the layering of medications
Consumer engagement is needed with all medications being prescribed to be fully empowered, to understand: 1) the need for prescriptions, why and when appropriate, 2) the side effects of medications to determine alternatives versus adding on more medications, and 3) to eliminate the misuse of medications without the continued layering of additional drugs. Antibiotics should only be used when the body, given time, cannot fight a severe bacterial infection. And, antibiotics should only be given out after a culture is performed to eliminate a virus as the cause, or to target the specific bacteria. Broad spectrum antibiotics should only be used with life threatening-septic issues while waiting for a culture, or there is not the ability to perform a culture.

A middle aged male was recently experiencing severe abdominal pain, subsequently prescribed three (3) medications in two (2) weeks from three (3) different sources (an Emergency Room, a primary care doctor, a Gastroenterologist). There was no diagnosis, no care coordination within an established plan of care, no thorough instruction in the medications, with the last prescription based on a guessed misdiagnosis which worsened his pain. One prescription was a steroid with the patient being instructed to take as he needed it; the second was an offering by the office secretary blindly asking if he wanted an Epipen when he called to actually speak with the physician for worsening abdominal pain, swelling and to discuss his lab work.
The common standard operating procedure (SOP) in medicine has become symptom and write a prescription, another symptom and write another prescription, etc. This SOP has lent to the opioid crisis, antibiotic resistance, as well as many other drugs being dispensed routinely with side effects causing secondary prescriptions for the side effects of the existing medications being taken.
Several variables cause the use of this SOP beginning with the lack to get a full, detailed history - taking time to speak with patients - to establish a diagnosis and then plan of care, determining if simple steps are first needed such as icing and therapy for pain before opioids, or to remove foods and medications isolating side effects or allergies. Last week, I attended the HIMSS conference, the largest healthcare conference in the country, with attendees from around the world. One executive stated, "I just returned from Finland where they have an effective health system, because people live healthy, and the doctors appropriately tell their patients NO when seeking a simple, quick fix of a drug that is not needed."
Reasons for the mainstream SOP?
I think there are always multiple reasons for issues within healthcare. The symptom=prescription issue can be: Doctors are processing patients through with 'factory-care', Physicians receiving kickbacks from pharmaceutical companies; The lack of proper clinical training; Protocols blindly being followed without individual evaluation (e.g. Vanderbilt University study on Plavix standard for all Cardiac Cath Patients); as well as the alliance of public policy and pharma, direct consumer marketing without proper education.
A healthcare executive summarized the situation well last week when stating to me, "I ultimately make the decision for my own care, with the advice of the physician. It is the doctor's role to diagnosis, and then we discuss all options, along with a plan of care, coordinated with speaking with all other involved physicians." It is important for consumers to understand the need to champion their own care working with physicians, determining what options should be used before medications (diet and some of the old fashioned home remedies still hold true), addressing underlying issues versus only symptoms, and removing or changing medications to eliminate side effects when there are alternatives. Questions to have answered:
An example of direct consumer marketing lacking in education: In 2016, there was broad publication when the company Mylan raised the prices of the Epipen after State Law was passed to stock it in every school. Many individuals and groups were upset because there is not a generic offering. With proper information, the public would be educated that Epipen is the patented delivery system, not the drug epinephrine. The generic already existed in the form of a $15-$18 sterile needle. It is also necessary to establish where and when is it appropriate to stock epinephrine, not specifically the Epipen.
Why are you prescribing this medication, what is it specifically doing in my system?
What are non-medication alternatives, what are other medication alternatives?
How long should I take this, what is the outcome? How does it interact with my other medications?
What should be monitored for an outcome, side effects?
| Dr. Lee Beecher and David Racer in their book Passion for Patients wrote, "Dr. Kübler-Ross … called me to her office … “Ach, you’ve got a problem.” She said I needed to more clearly communicate... You have to learn about how to be a good son-of-a-bitch.” Pritzker (medical school at University of Chicago) taught me how to be a problem solver ... No one told me what I had to believe or how I had to think. They taught me how to think and apply what I learned to help my patients." (pages 55-57) Today I read someone describing the Forbes article by Brent Gleeson, “Apparently, during SEAL training, peer reviews are a weekly event. They have a process called top five, bottom five. Every week you anonymously rank the top five performers in the class as well as the bottom five.” Unfortunately, with political correctness and mandating diversity in healthcare, leaders and peers cannot or choose not to do ranking and hiring based upon performance. I have seen in the health industry that no one is allowed to hurt a doctor/nurse's feelings because they are being incompetent or under-performing, with patient's lives at stake. | It is a wonderful idea of ranking on performance so everyone pushes each other to excellence. But when a 30 year veteran nurse is told to shut up because she was holding accountable the new doctors and nurses not performing, competency rating (especially by knowledgeable veterans) was a great practice that worked 20-30 years ago - but one that is not tolerated today. The result, medical errors are now the #3 cause of death. The industry is killing people with our focus on kindness versus caring competency. Personally, I want a well trained, experienced, compassionate son-of-a-bitch taking care of me, as opposed to someone who is being nice while not knowing what they are doing. I want a doctor and nurse who takes care of me so I can go home and I don’t have to see them again because they are my quality clinicians, not my pals. |
Elisabeth Kübler-Ross, Passion for Patients, (page 62)
Day’s statements exemplify an important component that has been lost in healthcare training - that of muscle, or specifically, movement memory. Clinicians are supposed to be trained in school regarding the need and proper technique for handwashing. More importantly, clinicians used to have extensive clinical time working in patient areas developing the movement memory for proper hand washing, and automatically keeping in mind what is clean vs. dirty, where established sterile fields are located with maintaining of sterile gloved hands. The training was extensive and repetitive, for clinicians to automatically move appropriately in fast paced, life threatening situations - to not have to think and just act. One common, simple example is the insertion of IVs for fluid administration or needles for drawing blood. The needle or IV cannula (the needle with covered sheath inserted into the vein) is sterile, with clinicians wearing nonsterile gloves. The skin is typically wiped with alcohol to clean, and then all too often clinicians press nonsterile gloved fingers on the cleaned skin to feel for the vein; thus, contaminating the cleaned surface of the patient’s skin where insertion directly into their vein will occur. Even though the nurse/doctor is wearing clean gloves, they are not sterile, and worn to protect the clinician. With repetitive movement training, clinicians would press to find the vein before properly cleaning the skin, and clean their gloved fingers at the same time as the patient’s skin.
Two frequent complaints often heard from patients, "They dug around in my arm and could not find the vein, it was so painful." "They poked me five times because they did not know what they were doing." Blood draws and starting IVs is a skill, just like shooting at a target or in high stress a gun fight, that requires proper training of technique, and more importantly, repetitive practice - especially with the understanding when someone's life depends upon it. Additionally, the conditioned good technique should be second nature to purge ALL air from needles and tubing, including from the side ports of IV tubing, to prevent the potentially fatal embolus as a hospital acquired condition (HAC).
With the great reduction of hands on clinical time in schools (with replacement of online theory, population/global health, writing, and shadowing nurses), this movement memory training has been lost, with the shift of cost to hospitals for training, buying expensive monitoring equipment, or addressing the subsequent HAIs/HACs. Bringing the ingrained, repetitive movement training back to school training would instill within clinicians and CNA/PCT caregivers the instinctual, reactionary awareness of dirty versus clean or sterile, and proper IV/needle insertion, while delivering care; whether normal daily care or imminent life versus death situations – because they just do what they are trained to do without having to stop and think through quality actions.
Ms. Rohloff, a 35-year healthcare veteran with experience in nursing, business and information systems, spoke with Becker's Hospital Review about providing consumers with more detailed evaluation of quality care delivery. [read more]
click an article
to read and post comments
Search topic
select category
All
APAC Teams
Care Quality
Champion Your Own Care
Clinician Quality Education
Experience Satisfaction
Healthcare Consumerism
Health Innovation
Medical Care Coordination
Palliative Care
Patient Engagement
Physicians
Population Health
Transitioning Care Coverage
search by date
July 2024
June 2024
April 2024
March 2024
February 2024
January 2024
November 2023
October 2023
June 2023
May 2023
October 2022
September 2022
July 2022
August 2020
April 2020
January 2020
June 2019
May 2019
April 2019
October 2018
September 2018
August 2018
July 2018
May 2018
April 2018
March 2018
February 2018
January 2018
December 2017
September 2017
June 2017
October 2016
September 2016
May 2016
March 2016
October 2015
June 2015