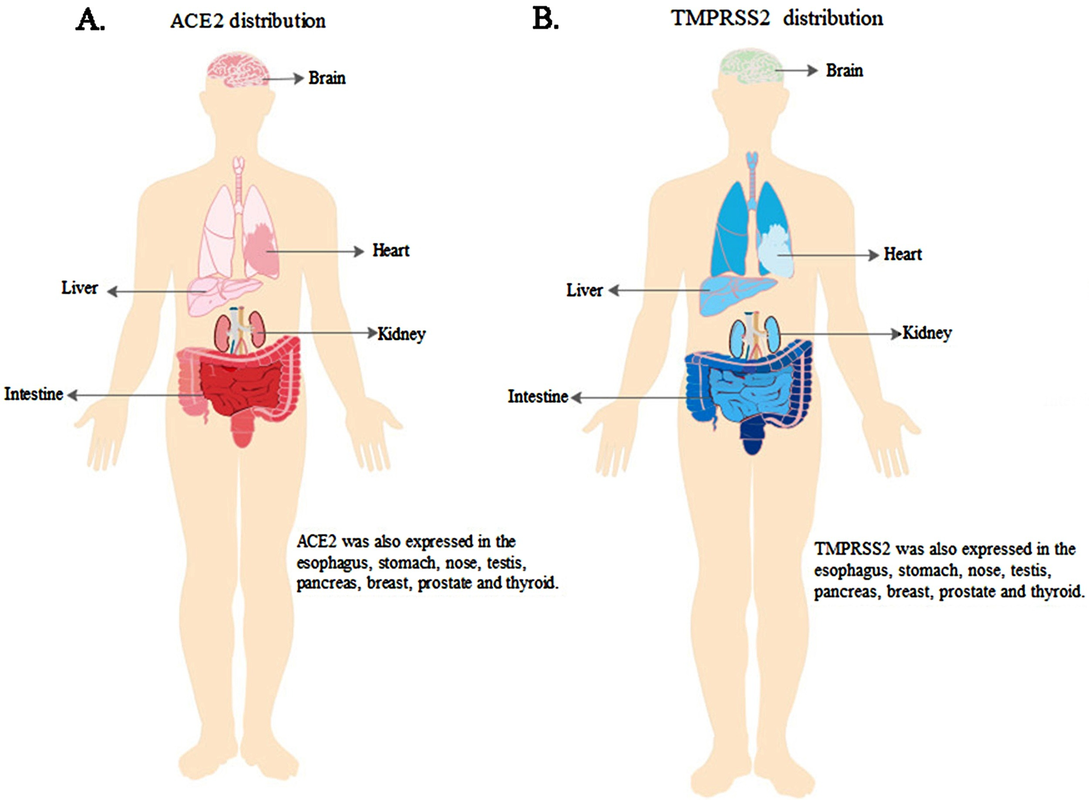
Compiled Rose Rohloff from input by Dr. Peter McCullough and Dr. James ThorpMany persons may have been illegally coerced into taking the Covid shots.(see blog entry regarding the 1974 National Research Act) The following is an extensive Spike Protein (SP-C) lab panel, sectioned into subpanels (a panel is a collection of several lab tests), for evaluating if you systems may have been impacted by the spike proteins - with or without existing symptoms. Note some individual labs may be duplicated in various panels and will not have to be duplicated. Champion your own care and consult with your choice of physician with informed consent. General Tests and Evaluation of Cardiac
The following evaluate antibody (Ab) in your blood, proteins made by the immune system to fight foreign bodies (bacteria, virus …)]**
For women of reproduction age
For autoimmune and/or bleeding issues
1No commercially available test for circulating spike amounts are available at this time and will update as one becomes available. Serum Spike Antibody (Ab) is the surrogate at this time. Higher spike Ab titer correlates with severity of infection/long COVID. Pathologists are able to determine if tissue spike is from Shots/Injections versus infection via correctly performed autopsy, as per Dr. Ryan Cole in deposition of case. “Normal” Value-ranges & Description of various testsSome parameters vary slightly based on which lab is used - low or high readings should be determined by the specific lab being used at the time of lab test, and for individuals regarding their baselines, underlying conditions. D-dimer CBC CRP CMP Various Antibody testing to determine if your immune system is or is not fighting off a foreign substance. TSH: ***
Amenorrhoea Panel
0 Comments
Who is in charge of healthcare? Is your Health insurance coverage invalidated/exempt? 5G and edc4/12/2024 by Rose RohloffEach individual should be in charge of their own healthcare decisions, safety surroundings, and be treated individually. So, a good question to ask, "Who actually is in charge?" Laws and Executive Orders (EOs) regarding healthcare under "public health"Created by Todd Calendar, Esquire H.R.3832 - Disease X Act of 2023 118th Congress (2023-2024) Open "disease" cart blanc for them to choose (or orchestrate?) ‘World Health Organization (WHO) Has No Authority to Dictate U.S. Health Policy’ factcheck.org March 2, 2023 "Although the accord is being called ... a treaty or another kind of binding agreement, such as the WHO Framework Convention on Tobacco Control, or a nonbinding agreement, such as the Paris Climate Accord. “As with all international instruments, any accord, if and when agreed, would be determined by governments themselves, who would take any action while considering their own national laws and regulations,” a WHO spokesperson told us." Federal and Local Governments would be in charge regarding any Rights violations. The accord is accumulation of monies $$$ to be "distributed" to various countries/persons, in the name of public health.
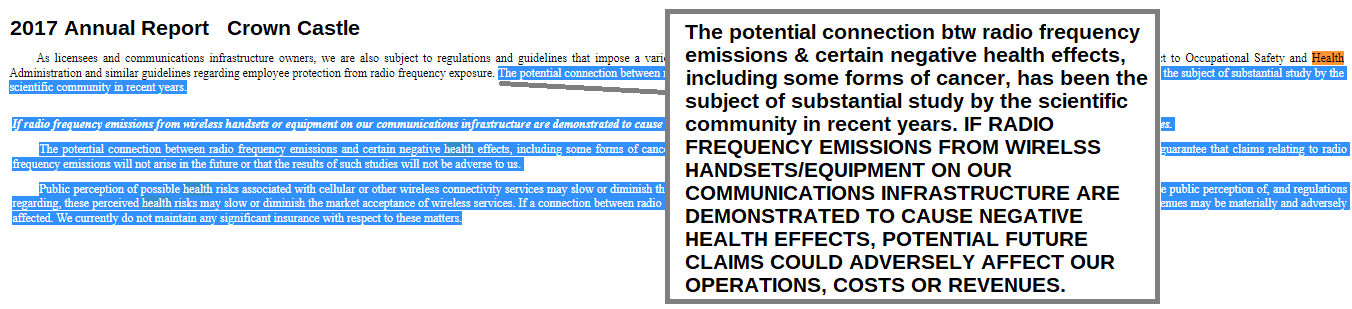
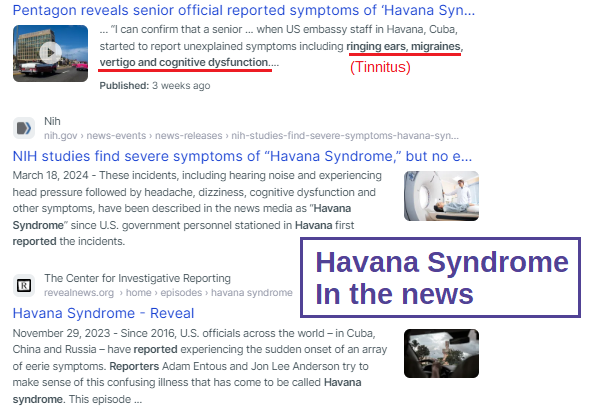
LTC (ret) Green Beret, Doc Pete Chambers, MD, bioweapons expertRisk of 5G rolled out, without safety studies, by Federal, State and Local governance. Communities were not asked regarding rollout, or informed regarding safety issues of 5G. Are we experiencing history repeating the dangers of DDT, Asbestos, many FDA "approved" drugs recalled because they lacked safety, etc.?
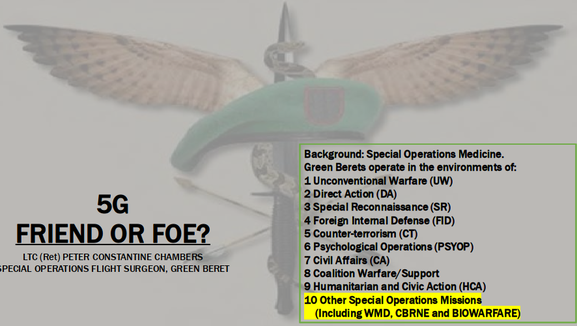
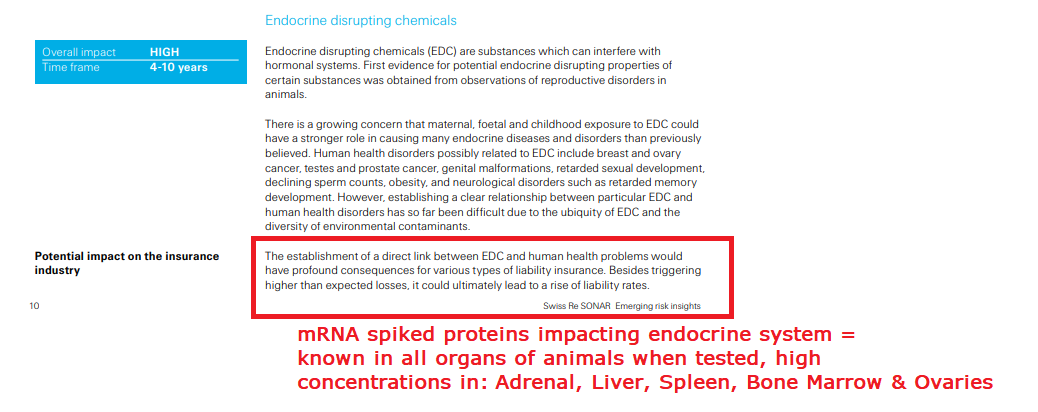
Are individual healthcare insurance policies, the underwriters of policies, being invalidated without the knowledge of people, and against their choice - through lack of knowledge, lack of informed consent, and through illegal coercion? Electromagnetic RadiationEndocrine Disrupting Chemicals (EDCs)by Numerous expertsMy desire is to provide several articles from those adroit in the subject. COPPER: the less talked about, and important trace mineral, the importance of Zinc, and when taking high Zinc, make sure you know the ratio of zinc to copper supplements.
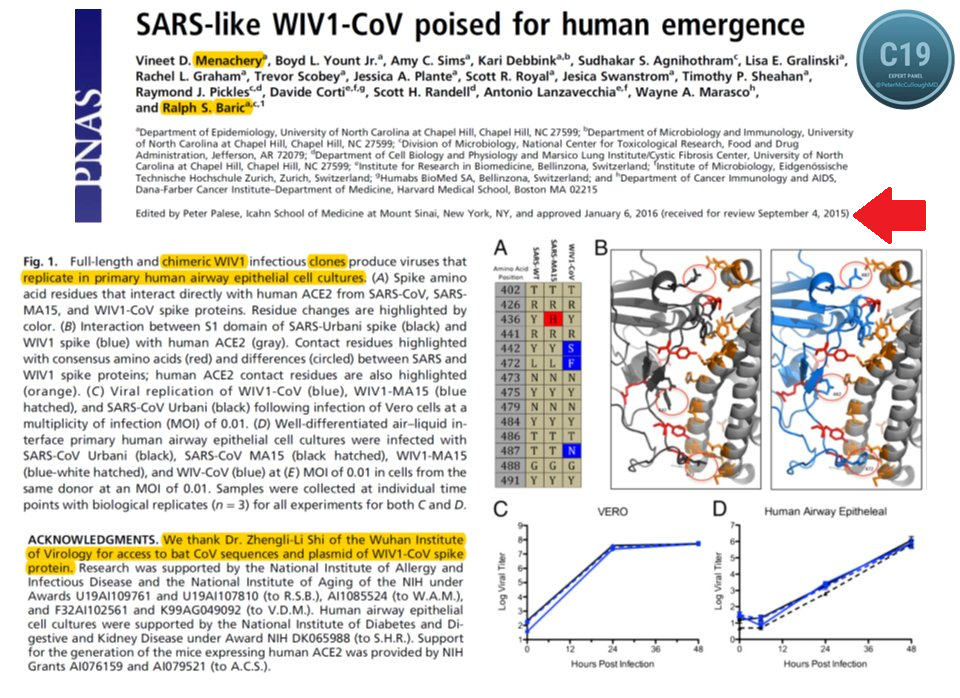
Ralph Baric and other scientists knew in 2010 the "antidote"/treatments for the upcoming virus(es). He coauthored the discovery "Increasing the intracellular Zn(2+) concentration with zinc-ionophores like pyrithione (PT) can efficiently impair the replication of a variety of RNA viruses". Dr. Vladimir Zelenko based his effective protocol after watching the "MedCram Lecture 34 by Dr. Roger Seheult about the use of zinc and zinc ionophores. Zinc is an essential mineral for humans, and a little extra zinc is sometimes used to lessen the intensity of colds and sore throats. An ionophore is a chemical that opens the cell wall to allow minerals (ions) to enter. ‘First do no harm’ Zinc is an over-the-counter supplement. Hydroxychloroquine (HCQ) is a reliable ionophore, and it has a well-established dosing regimen and safety profile." Zinc ionophores "increase the intracellular concentration of Zinc ions causing significant biological effects. Review ionophores: HCQ, EGCG (a plant compound particularly prominent in green tea) and Quercetin (particularly in citrus fruits, apples, onions, parsley, sage, tea, and red wine. Olive oil, grapes, dark cherries, and dark berries such as blueberries, blackberries, and bilberries are also high in quercetin and other flavonoids.) "
Mount Sinai "Copper is a mineral that is found throughout the body. It helps your body make red blood cells and keeps nerve cells and your immune system healthy. It also helps form collagen, a key part of bones and connective tissue. Copper may also act as an antioxidant, reducing free radicals that can damage cells and DNA. Copper helps the body absorb iron. Your body also needs copper to make energy."
Dr. Shiva The Power of Copper to fight virus, bacteria on contact
Copper has even been shown to be very effective at exterminating the much-dreaded hospital ‘superbug’ MRSA. In tests sponsored by the Copper Development Association, a grouping of 100 million MSRA bacteria atrophied and died in a just 90 minutes, when placed on a copper surface at room temperature. The same study found that the same number of MSRA bacteria on both steel and aluminium surfaces actually increased over time. On looking at these figures, many scientists have concluded that the installation of copper-based fixtures such as taps, light switches, door handles, door knobs, pull handles, and push plates in areas such as hospitals could save thousands of lives each year.
Professor Bill Keevil, head of the microbiology group at Southampton University, added his voice to the growing scientific consensus behind this by advocating the use of Copper and Brass door furniture, fixtures and fittings in public places and on public transport, as they could dramatically cut the threat posed by superbugs. In research published in the journal Molecular Genetics of Bacteria Professor Keevil wrote: “There are a lot of bugs on our hands that we are spreading around by touching surfaces. In a public building or mass transport, surfaces cannot be cleaned for long periods of time… Until relatively recently brass was a relatively commonly used surface. On stainless steel surfaces these bacteria can survive for weeks, but on copper surfaces they die within minutes… We live in this new world of stainless steel and plastic, but perhaps we should go back to using brass more instead.” In addition to direct contact killing of bacteria and harmful microbes, amazingly Copper surfaces have been found to exude an antimicrobial 'halo' effect on surrounding non-copper surfaces. Research in the intensive care unit a Hospital in Greece found that other surfaces up to 50 centimetres from copper surfaces experienced 70% microbial reduction, compared to the same surfaces with no proximity to copper-based materials. The ‘Halo’ effect was also observed in trials at a U.S. clinic in 2010. This amazing effect demonstrates just how powerful copper is as a weapon against bacteria." www.morehandles.co.uk by Rose Rohloff
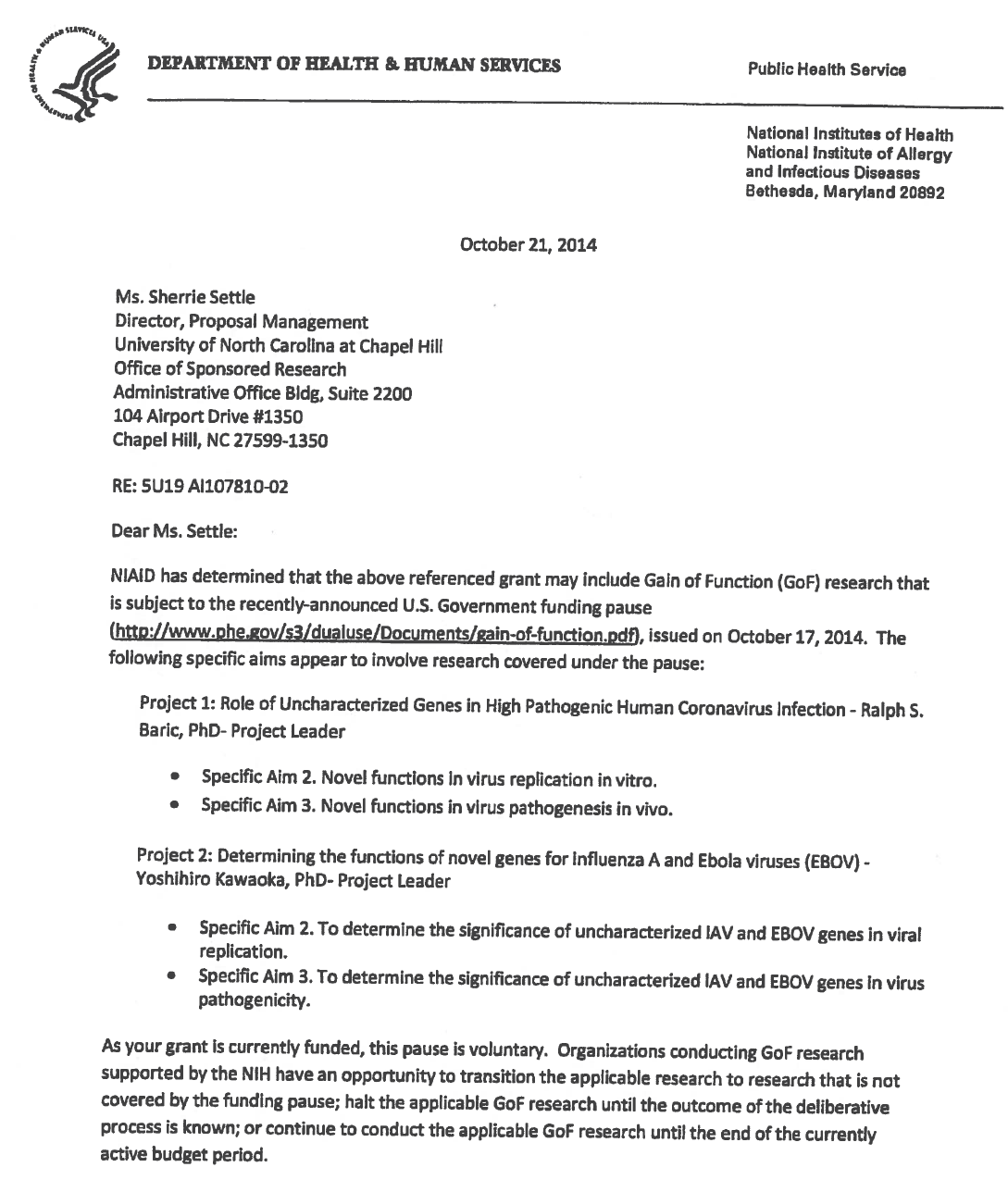
* Date: written 2015 posted 2016
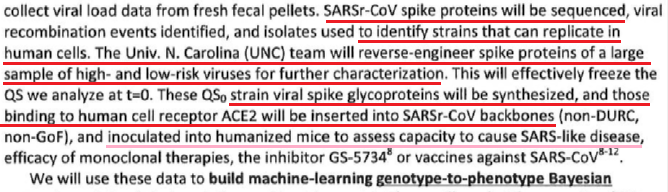
* Not natural: chimeric infectious clones, GOF
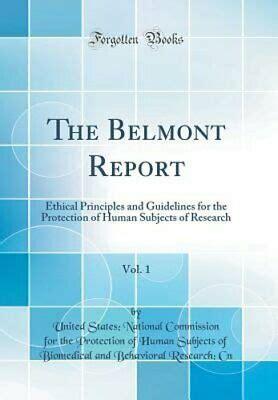
The 1974 Research Act was created in entirety from the Belmont report, and put into place to prevent the Government, it agencies or representatives, military and private companies, from violating an individual's freedom: by forcing, tricking or coercing persons for research, testing and administration of unknown injections/materials, and experimental procedures. This law was enacted after a century long track record of precedence including, and not limited to, the following:
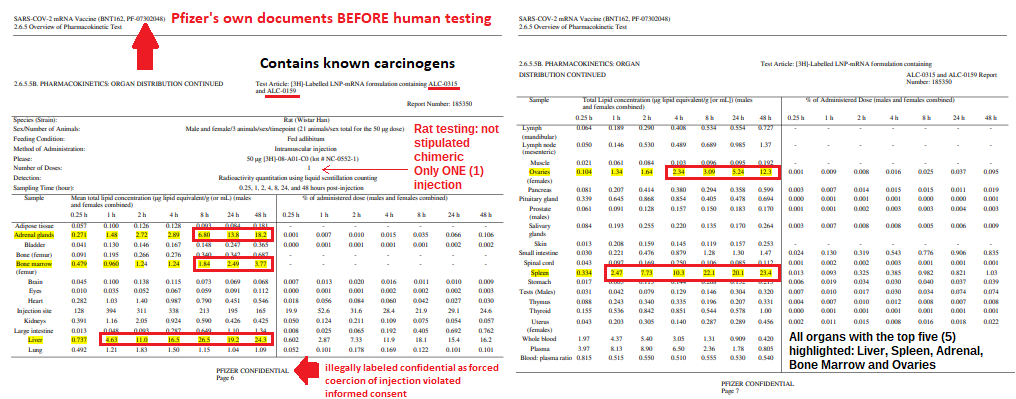
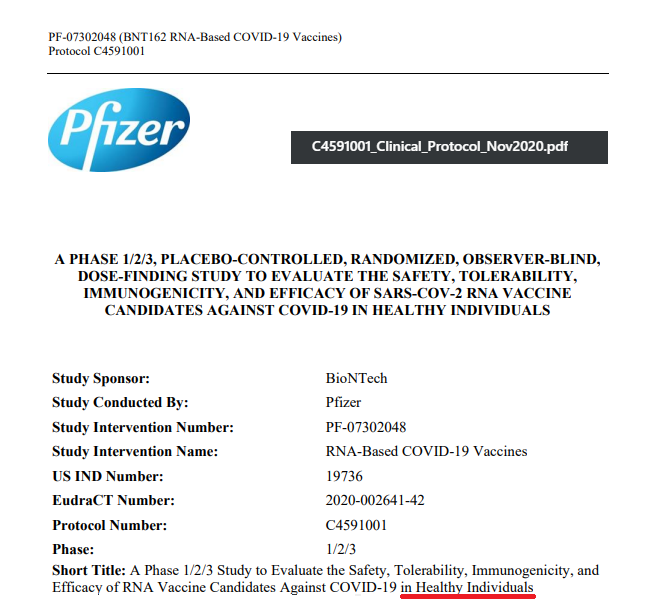
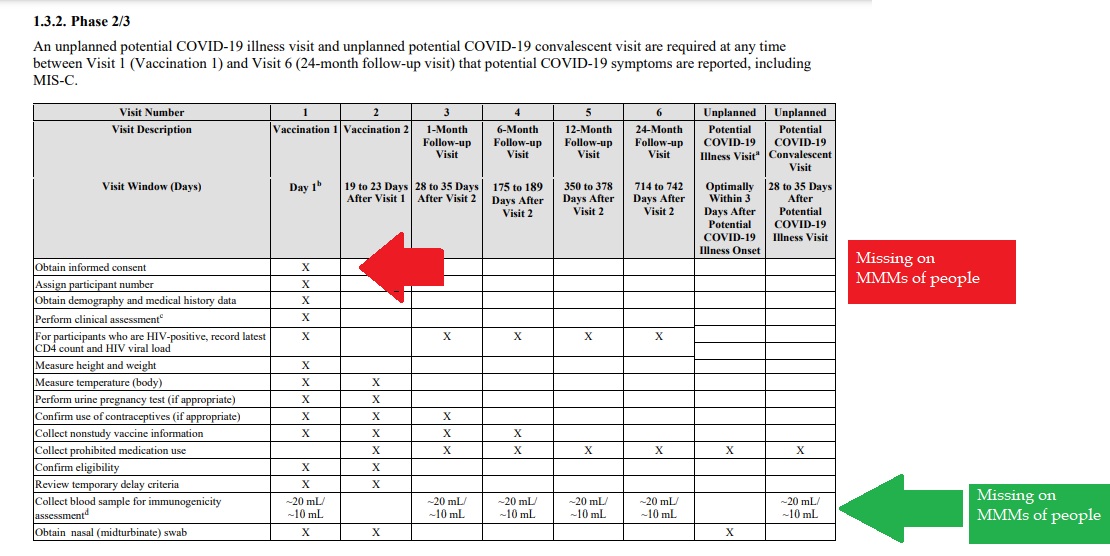
Demonstrated lack of Respect for Persons and their protections in violation of 1974 law. 1- Autonomous agents, individuals capable of deliberation about personal goals and of acting under the direction of such deliberation. The Government and companies have to give weight to autonomous persons' considered opinions and choices, and cannot obstruct their actions and judgments, nor deny individual freedom to act on considered judgments, and cannot withhold information necessary to make a considered judgment. Necessary information includes - but not limited to - all medical opinions by established, industry experts, health status, the necessary assessments, labs, with close monitoring of physical lab and test follow ups of each and every autonomous persons as part of clinical research and testing, along with full documentation of testing, efficacy, use of chimera for research and testing, any and all conceivable side effects, and interactions of conditions. 2- persons with diminished autonomy are entitled to added protections. Violators to the law have been marketing to the most vulnerable, including the immature and the incapacitated who were in need of extra, added protections, even to the point of excluding them from any injections or procedures which may harm them; violating added safety precautions for children, elderly, or those with diminished capacity. Informed consent - must include full disclosure of ALL contents to be injected, any and ALL possible side effects (which can be several pages long), how those persons are individually to be closely monitored, safety guidelines, and above all the right to say no before or at any time, and full reporting of all individuals regarding their safety monitoring/labs/assessments, and any and all side effects. By promoting COVID shots all still under clinical trial/research, and coercing with careers/jobs, inability to travel, etc. in order to take the shots, this law is being violated through: lack of informed consent, lack of protections of autonomous persons, and/or illegally acting as IRB safety board members marketing to those not autonomous and capable of self-determination, with higher standards of protection to be invoked, and assuming the role for their safety. The maxim "do no harm" has long been a fundamental principle of medical ethics. Claude Bernard extended it to the realm of research, saying that one should not injure one person regardless of the benefits that might come to others. An agreement to participate in research constitutes a valid consent only if voluntarily given. This element of informed consent requires conditions free of coercion and undue influence. Undue influence also includes offers of an excessive, unwarranted, inappropriate or improper reward or other overture in order to obtain compliance. Also, inducements that would ordinarily be acceptable may become undue influences if the subject is especially vulnerable as in the case of targeting children, persons with limited capacity, and elderly with elements of mental defect, or instilling fear. Short term morbidity and mortality cases from the shots are well reported and known, such as death, myocarditis along with spontaneous cardiac arrest with no warning, debilitating neurological conditions, etc. And, there is no means yet to determine mid and long term effects because Phase I trials have not been competed, let alone Phase II and III - which is vital information in order to determine informed consent. Injustice has been performed with companies and government representatives, by involving vulnerable subjects, including the young, those unable to fully comprehend with all necessary information, and scaring parents with compromised capacity for free consent. In addition to lack of individual, tightly scheduled, continual monitoring and follow ups, autopsies of all persons involved in this trial participation should be conducted for reporting by the pharmaceuticals companies for any and all persons who received the shots, as well as labs determining efficacy and detriments (as examples, antigen creation, D-dimer, Pulse Cardiac and Troponin Tests) for all those who were coerced or unduly influenced to participate in research. This law was created to protect people from government abuse through experimentation. The government cannot arbitrarily dismiss components, create resolutions or stipulations to supersede the law, as to invalidate its protection of individuals from them, including, but not limited to Health and Human Services (HHS) Center for Disease Control (CDC), Food and Drug Administration (FDA), National Institute for Health (NIH), etc. and pharmaceutical companies, etc. Persons have been illegally acting as members of, or bypassing, IRB safety review and monitoring of each and every person receiving injections, with open undue influence and coercion, to participate in Covid injections. Coercion has been especially directed to the diminished autonomous, children and elderly, through TV ads, library recordings, verbal encouragement, schools or other public venues acting as government agents, and/or clinical researcher recruiting participants, and/or illegally as untrained IRB member who is not following up to ensure safety of the people they recruited, coerced or used undue influence. Overall lack of informed consent has become too often common practice across the healthcare industry, including people being given consent forms hours or minutes prior to surgery; no alternative treatments or lifestyle-nutrition changes prior to medications begin prescribed, and undue influence to intubate or perform surgery on patients in lieu of alternative treatments.
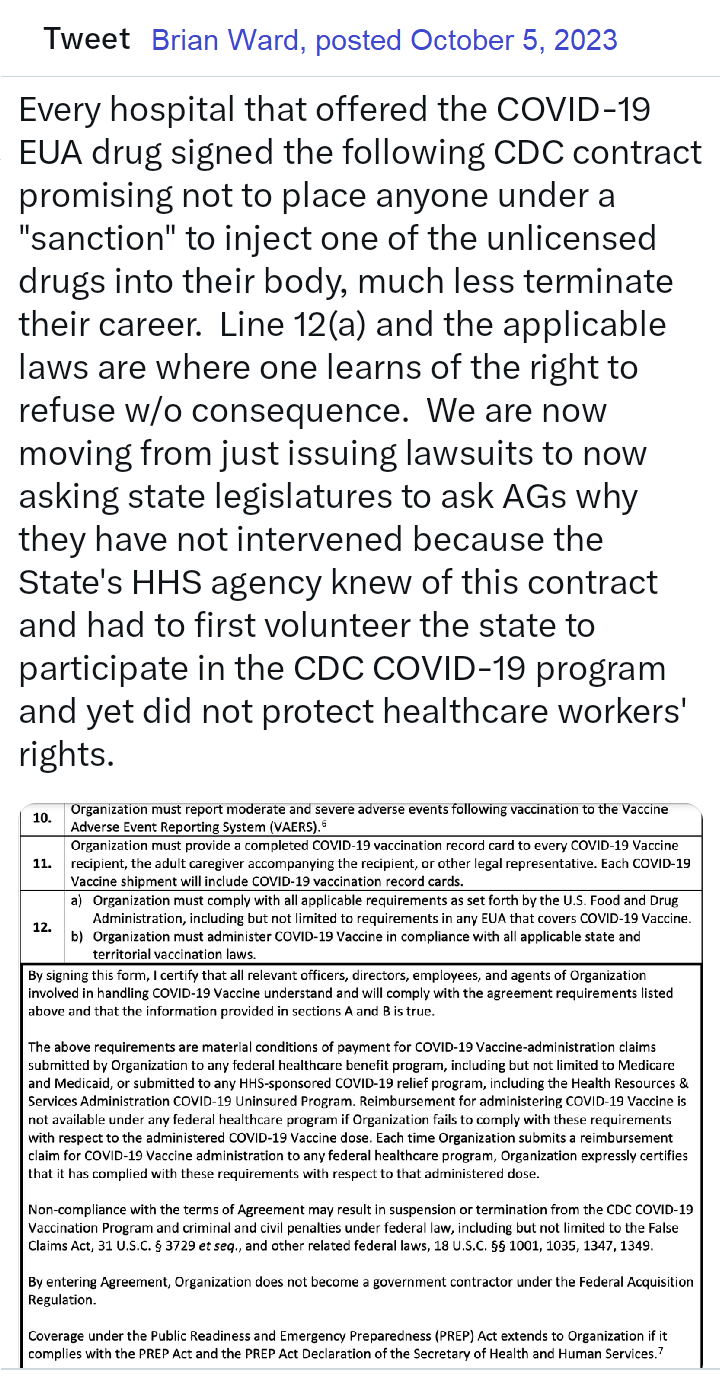
Lawsuits for unconstitutional violation of laws regarding shotsPosted by Brian Ward on Twitter Guess what? Defendants in our lawsuits no longer argue that they had a right to mandate EUA drugs due to their state's at-will employment doctrine. That the EUA drugs can be mandated. That they had the authority to even issue the mandate. Why? Read the 127 pages, and then you'll understand that it was a legal lie from the beginning, but due to the novelty of the laws, no one knew of them. As courts have stated, "sometimes laws take naps," and these laws never showed up for work until now. https://coloradomedicalfreedom.com/wp-content/uploads/2023/08/Stamped-Final-Complaint.pdf full document https://coloradomedicalfreedom.com/wp-content/uploads/2023/08/Stamped-Final-Complaint.pdf page 127 C. the Secretary has no “authority to require any person to carry out any activity that becomes lawful pursuant to an authorization under this section…” 549. In 2005 Congress passed the PREP Act94 which provided the following regarding preemption of state law: (8) During the effective period of a declaration under subsection (b)…no State or political subdivision of a State may establish, enforce, or continue in effect with respect to a covered countermeasure any provision of law or legal requirement that— (A) is different from, or is in conflict with, any requirement applicable under this section; and (B) relates to the…administration…of the covered countermeasure, or to any matter included in a requirement applicable to the covered countermeasure under this section or any other provision of this chapter, or under the Federal Food, Drug, and Cosmetic Act [21 U.S.C. 301 et seq.]. 550. Therefore, via the PREP Act and 21 U.S.C. §360bbb-3, Congress expressly prohibits Defendants from: A. interfering with the authority of the Secretary, B. establishing a condition not authorized by the Secretary, C. establish conditions contrary to the Secretary and the congressional statute under 21 U.S.C. §360bbb-3, D. mandate participation in any 21 U.S.C. §360bbb-3 product or PREP Act activity, E. interfere with an individual considering participation in a 21 U.S.C. §360bbb-3 product or PREP Act activity, F. penalize a person refusing to participate in a PREP Act product or activity or 21 U.S.C. §360bbb-3 product. 551. The executive branch of the United States Government purchased all COVID-19 licensed and EUA drugs using federal funds. Congress expressly prohibits the federal government Brian Ward @GodsRiddles Nov 1, 2023 Breaking…Gov Gavin Newsom and Kaiser have been sued in federal court for requiring healthcare workers to inject an experimental drug into their bodies as a condition to sell their labors in the marketplace. The requirement violated the workers’ Equal Protection of Laws and Due Process rights. Moreover, Kaiser signed a contract with the CDC promising not to mandate participation but did so anyway. Kaiser and Newsom fraudulently concealed the fact that nurses would be required to forfeit litigation rights if they incurred an injury from the use of the experimental drug. The California Nurses union stood by and refused to stop Newsom’s tyranny, leaving members without representation. Governor Newsom perpetuated the greatest assault on the US Constitution in the state’s history and the CA AG did nothing to prevent it. Worse yet, is that CA and Kaiser already had an agreement with HHS promising to never place an individual under a sanction for refusing to inject federally funded experimental drugs into the body. Legal Fact: medical providers have dual roles in relation to their employees. An employee can be a patient and an employee. Should a hospital mandate the use of a drug under the PREP Act as a condition of employment and the patient is injured then the patient would find it difficult to sue the medical provider for that injury. However, the employee has the right to seek compensation irrespective of the PREP Act because it’s an on the job injury. Of course this opinion does not account for the laws of all 50 states but demonstrates why one should seek legal advice immediately upon sustaining an injury. This is not my opinion but the chief judge of the 11th circuit who wrote a slip opinion when he was AL AG denoting the company is liable for vaccine injuries because the company believes the vaccine would benefit the company. Last edited10:55 AM · Nov 10, 2023
Brian Ward - Twitter Oct 25, 2023 Legal Fact: Any state that penalized citizens or denied unemployment benefits to an individual terminated for the sole reason of refusing to inject an unlicensed investigational drug into their body violated the individual's Fourteenth Amendment Equal Protection and Due Process rights. The U.S. Congress conferred legal authority onto an individual to either accept or refuse an EUA product. Both options were enacted by a valid act of Congress and must be equally protected. Moreover, the Supremacy Clause of the Constitution denied that state authority from interfering in the chosen option. The state established what courts call an Unconstitutional Condition. SCOTUS said: "But the power of the state in that respect is not unlimited; and one of the limitations is that it may not impose conditions which require the relinquishment of constitutional rights. If the state may compel the surrender of one constitutional right as a condition of its favor, it may, in like manner, compel a surrender of all. It is inconceivable that guaranties embedded in the Constitution of the United States may thus be manipulated out of existence." Governors and state agency directors violated their oath of office & the Constitution the moment they required COVID-19 EUA participation and or penalized an individual's federally protected option. They deprived citizens of their interest in liberty and property and, unfortunately for some, their very lives, all without due process. They did so by applying the law unequally demoting those who refused to that of a second-class citizen. Legal Fact: 21 U.S.C. §360bbb-3 and the PREP Act expressly restrict public and private employers from conditioning access to employment and other benefits upon a person injecting an FDA-classified experimental drug (Pfizer-BioNTech COVID-19 Vaccine) into their body. The CDC stated, "Coverage under the Public Readiness and Emergency Preparedness (PREP) Act extends to Organization if it complies with the PREP Act and the PREP Act Declaration of the Secretary of Health and Human Services." "IF IT COMPLIES" is the key phrase here. When a governor issued a proclamation that directly violated the federal statute, the governor did not comply and fraudulently amended the federal law in violation of the Supremacy Clause. The PREP Act and 21 U.S.C. §360bbb-3 provide a legal right to individuals considering participation in the product/activity. That legal right is the option to accept or refuse. Therefore, the immunities provided to persons participating in activities under the PREP Act extend only so far as they do not force persons to participate in the product/activity. Governors, employers, hospitals, all FORCED (under threat of a penalty) individuals to participate in violation of federal law. Force does not have to mean physical force. It can be the force of law, rule, or other means having the same negative effect as physical force. The courts have said that force means to prevent a person or cause a person to participate in an activity outside of their free will and voluntary consent. Significant lawsuits inbound! 12:45 PM · Aug 29, 2023 Brian Ward Aug 2022 BREAKING: LA Superior Court requiring LAPD to reinstate an officer terminated for refusing the vax mandate. Full back pay too! This is under a Writ of Mandamus, which is rare. Legal Fact: "Nothing in this section (EUA Law) provides the [HHS ] Secretary any authority to require any person to carry out any activity that becomes lawful pursuant to an authorization under this section, and no person is required to inform the Secretary that the person will not be carrying out such activity." - The Secretary may grant access to an unlicensed drug (Pfizer-BioNTech COVID-19 Vaccine) during an emergency but he can not mandate that anyone manufacture, distribute, store, administer, or receive the product. His authority is non-transferable, nor may he delegate it to another person. Therefore, by what authority are universities and private employers mandating that which Congress prohibits? EUA drugs are "controlled" drugs by Congress, and no person may participate in them outside of the conditions established by Congress. Moreover, Congress expressly prohibits private employers from interfering with your choice of accepting or refusing participation in the product. It was illegal - It is illegal - and it is being remedied in court. We will not allow this September to be a repeat of years past. 2:18 PM · Aug 21, 2023 Legal Fact: 100% of all hospitals and nearly all universities signed a FEDERAL agreement to abide by the ethical principles of the Belmont Report, though few know it, ANYTIME they involve a human with an investigational medical product such as any available COVID-19 drug. The report is only 10 pages long, but it holds in part: (1) Respect for persons incorporates at least two ethical convictions: first, that individuals should be treated as autonomous agents, and second, that persons with diminished autonomy are entitled to protection. The principle of respect for persons thus divides into two separate moral requirements: the requirement to acknowledge autonomy and the requirement to protect those with diminished autonomy, (2) To show lack of respect for an autonomous agent is to repudiate that person's considered judgments, to deny an individual the freedom to act on those considered judgments, or to withhold information necessary to make a considered judgment, (3) Respect for persons requires that subjects, to the degree that they are capable, be given the opportunity to choose what shall or shall not happen to them. BONUS ROUND - All US States and Territories signed this agreement pre-pandemic too. Yup, no one knows this either, including state attorneys general. Lastly, unlike the Nuremberg Code, the Belmont Report has the force of law via federal statute and contract. Last edited9:28 PM · Aug 2, 2023 Brian Ward via Twitter
The VERY first EUA issued was in 2005 for the Anthrax investigational drug for service members and civilian employees of the DoD. The EUA stated: A. Individuals (service members and civilians) who refuse anthrax vaccination will not be punished. (Emphasis added) B. Refusal may not be grounds for any disciplinary action under the Uniform Code of Military Justice. C. Refusal may not be grounds for any adverse personnel action. Nor would either military or civilian personnel be considered non-deployable or processed for separation based on refusal of anthrax vaccination. D. There may be no penalty or loss of entitlement for refusing anthrax vaccination, E. This information shall read in the trifold brochure provided to potential vaccine recipients as follows: You may refuse anthrax vaccination under the EUA, and you will not be punished. No disciplinary action or adverse personnel action will be taken. You will not be processed for separation, and you will still be deployable. There will be no penalty or loss of entitlement for refusing anthrax vaccination. Nothing in law has changed to negate the authority of DoD members to refuse EUA COVID-19 drugs except the 6 civilian appointees engaged in willful misconduct against our Armed Forces. 11:51 PM · Sep 3, 2023 Listen with this link https://thehighwire.com/ark-videos/aaron-siri-gives-testimony-on-the-floor-of-arizona-state-senate/ FDA working in support of pharma - no clinical trial testing of vaccines with "circular approval."
by Rose Rohloff
Calm intelligence, professionalism, logic and sense. Nine (9) doctors interviewed https://www.bitchute.com/video/2JPy7qZiXvNr/ regarding Covid, Hydroxychloroquine (HCQ) and masks. by Rose Rohloff
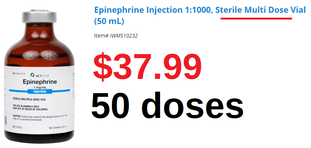
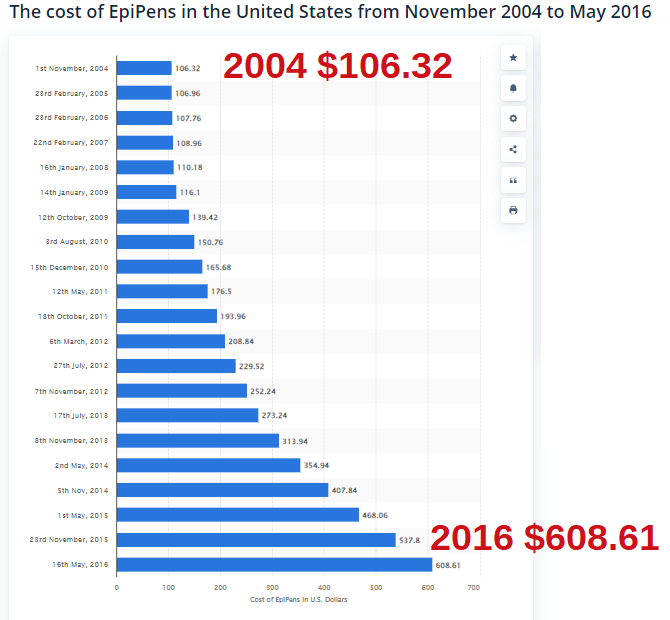
Use Case: A police officer was having hives and went to an emergency room. The staff asked him if he wanted an EpiPen. His response, "What the hell is it? The staff did not educated him, provide one to him to use if he felt he needed it. I informed him to read the fine print = it was a dose for a child an not a grown 200lb man, with an expiring date in a couple of weeks.
Summary
by Rose Rohloff |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
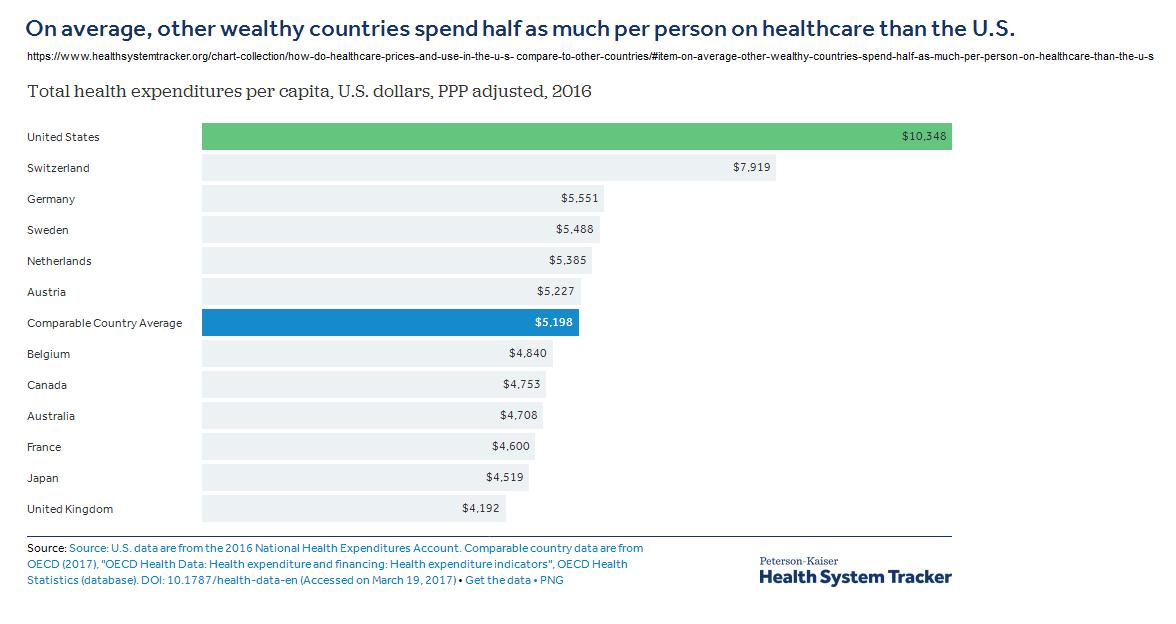
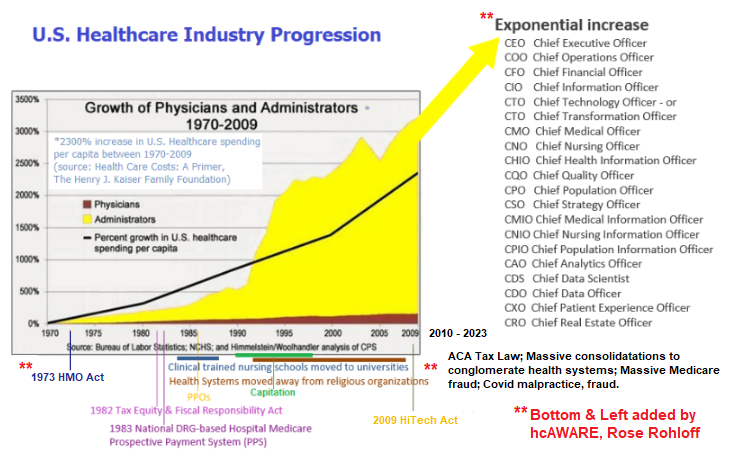
| Value is a relative term based upon personal perception, and oftentimes great marketing. True value is based upon insightful knowledge of what entails quality along with the cost of delivering goods and services. Value-based care is the new buzz for basing reimbursement in the healthcare industry. But again, what is value care: personal perception, marketing, cost? |
The primary issue with such score deviations is determining if poor marks are isolated instances (one offs); or, if the variance of only highest and lowest reflect the knowledge of reviewers. Are the high ratings from non-healthcare persons based on perception of the veneer friendliness and scheduling, with one star comments based on specific quality requirements, care competency posted by those with healthcare insight/experience?
As a 35+ year healthcare veteran, an answer was determined accompanying a Medicare patient ‘John’, in his mid-80s who experiences early stage dementia, to the office for a post-op visit for a leg stint placement.
| Upon arriving, another elderly patient (80s) was sitting outside, unattended in wheelchair, hot sun, 100 degree weather, no water. When asked why he was there, he stated, “I can’t stand the freezing air conditioning inside while waiting for a ride.” After walking John into the lobby, the gentlemen clearly seen through the glass door was pointed out to the receptionist stating that he was left in hot sun, no water, unattended. The receptionist stated, “It is his choice to stay out there.” I then stated, “Get someone to check on him, give him water, put him in the shade and check when his ride is supposed to arrive and monitor him if it is delayed or bring him inside.” One person escorted us back to exam room. She did not introduce herself or her title. She proceeded to take the blood pressure with no other vital signs (unknown if a secretary, an aide, a nurse or tech). She then asked the patient, “How much do you weigh?” He gave a number. As patient champion I responded, “He doesn’t know, he has not weighed himself. You need to weigh him yourself.” She responded, “We don’t have a scale.” She then left. I followed her witnessing her documenting the incorrect data. | I reiterated he has dementia with no idea how much he weighs. She replied, “It doesn’t matter anyways, we just need to put something in the record.” She was reflecting an 11 pound weight loss from previous recording. It is unclear if they performed the previous weighing, if it was done just prior to surgery to determine proper anesthesia delivery for his surgery. Another woman in scrubs entered the exam room without introducing herself or her title, asking John to remove his shoes and socks. (The scheduled appointment was with the PA so the patient assumed her identity.) She asked him if his wound was healed and he replied, “Yes.” She documented something in the chart without ever assessing his wound for healing or determining if there was infection. She bent down and felt his feet with her whole hands stating they feel warm, and then asked if he had numbness in his feet. John responded, “Yes.” | Having worked as a registered nurse (RN) in cardiovascular and neuro intensive care units (ICUs), I know she never did pedal (foot) pulse checks x4 comparing both feet. She never assessed location of numbness, or if chronic/intermittent, positional with sitting/, standing, walking, etc. The family had asked if aspirin could be stopped as the patient has experienced nose bleeds in the past. The staff person responded yes and since there was 90% blockage of the previous stint, it was cleaned out and continue Plavix. There was no establishment of lab work as part of care plan determining effectiveness of the medications, especially since the previous stint occluded. "1,750 or so stent patients are also prescribed Plavix to prevent clots from forming around the stent, but of that group, approximately 500 (29%) carry a genetic variation that prevents them from converting Plavix into its active form. This gene-related lack of response stands to be "especially severe" in about 50 (3%) of those patients, who won't derive any benefit from Plavix - 2010 Vanderbilt Medical Center |
Perceived value based on quality versus true value and cost
The care competency and quality as true value-based care during the visit includes:
- lack of basic cleanliness standards with severe cross contamination practices
- no introduction of name or title of any staff member
- fraudulent documentation in the electronic medical record (EMR)
- no assessment performed during a specific post operative visit (a family member could have taken the BP and said his feet felt warm.)
- lack of care planning and evaluation of medication regime
- unnecessary secondary office visit charging for follow up
- another elderly patient left unattended in the hot sun
If the U.S. healthcare system wants to achieve true value-based care, we need an educated population, higher accountability of staff standards with the ability to send evaluations direct to payers based on specific facts and not emotion, and surveys must include care competency reviews versus only veneer questions of politeness, room appearances, and on time scheduling.
Mayo Clinic Launches $1B Upgrade To Electronic Records System
CBS Minnesota 7/13/2017
Mayo Clinic defends executive raises
Molly Gamble (Twitter), Becker's Hospital Review 12/8/2022
Financial hits brought on by the COVID-19 pandemic in 2020 left many Rochester, Minn.-based Mayo Clinic executives taking small pay cuts. Compensation for CEO Gianrico Farrugia, MD, dropped 1 percent, for instance.
The next year, Mayo returned to raise executive pay, with a total of 26 employees reporting compensation of more than $1 million in 2021. That tally is up from 23 in 2020 and 21 in 2019.
In 2021, Dr. Farrugia's compensation increased by 27 percent to $3.48 million. Then-Chief Administrative Officer Jeff Bolton's compensation increased by 24 percent to $2.11 million. Kent Thielen, MD, CEO of Mayo Clinic in Florida, saw his compensation increase by 20 percent to $1.79 million and Richard Gray, MD, CEO of Mayo Clinic in Arizona, saw his compensation increase 26 percent to $1.78 million in 2021.
| As the dark side of IVF slowly comes into focus, even more transparency is needed by Pamela Mahoney Tsigdinos, July 27, 2018 |
The June 29, 2018 BECKER'S Hospital Review article shares the viewpoint "Froedtert CEO Cathy Jacobson: Not every patient needs a primary care physician" (PCP). The article is the perspective from the viewpoint of a health system CEO. The following is a perspective, counterview from patients, the individuals in the population.
Many people have expressed utter frustration from lack of a good Primary Care Doctor, warranting unnecessary ER visits because a doctor will not call back; the lack of one doctor in charge who would simply LISTEN to them, who knows them - not as personal friends, but with an in-depth professional relationship.
I have been asked several times in various states, "Do you know of any good Primary Care Doctors? I cannot find one." Universally, I am hearing: a gross lack of comprehensive assessments from doctors; clinicians not taking the time to get to know and listen to what is going on, causing the passing through of patients to specialists versus a primary care doctor creating a plan of care and focused tests for getting an actual diagnosis; lack of avoidance for hospital visits with increasing costs that could and should be avoided because conditions allowed to worsen; and doctors simply writing prescriptions for symptoms.
Her quote continues, "... insight further into consumer driven wants, we are finding that a substantial sector of the population does not want or need a primary care physician relationship. People need primary care but not necessarily a physician relationship." The issue is the primary care physician practices have been acquired by the hospital-health systems, with the biggest complaint from people in the population not being able to find a PCP; and those now under health systems, the doctor only giving 10-15 minutes of time, before passing off to specialists with no plan of care, and/or simply writing another prescription. Many in the public just find it faster, or are being told to just go to the ER. From the perspective of health system CEOs, it would appear primary care is not wanted or needed, which drives up the hospital ER and inpatient business. When actually speaking with individuals across the country, it is the opposite, people complain lack of care coordination, and "the doctor doesn't know me and is not taking the time to listen to me - I want them to actually figure out a diagnosis of what is wrong."
Kyle Reyes, CEO, The Silent Partner Marketing
The solution is bringing analysis down to the most base level of management with front line analysis, to coincide with first-hand observation, the voice of the patient & their caregivers/champions, and reducing the ever growing administrative overhead. Bigger is not better for addressing health and care of populations, when the focus is shifted upward with large systems where individuals are lost: Especially when the individual issues are indicative of the core problems that need to be addressed for quality care delivery.
The need for P&P Reviews
by Rose Rohloff
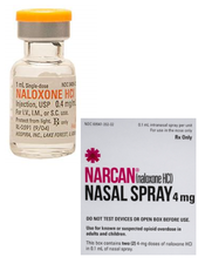
This week, reports were released in the media that US homes need Narcan to aid in opioid overdose epidemic, surgeon general advises
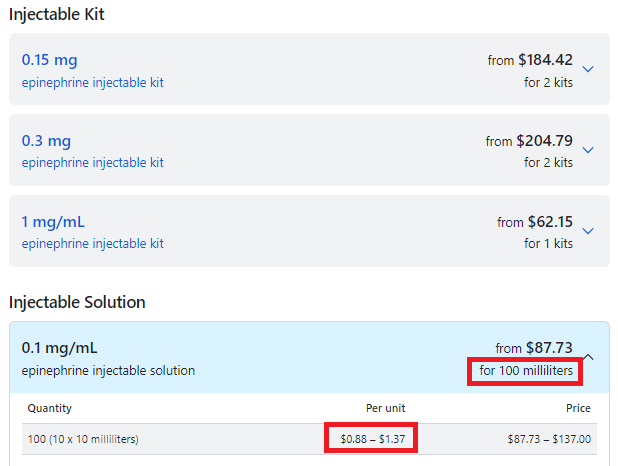
The general public needs to be aware: Naloxone has been reported to foster increased abuse of drugs by allowing revival of overdosing for continuing to take more drugs. Naloxone is the generic of Narcan. Just as EpiPen is only the delivery system and not the generic drug Epinephrine, It is important to know the difference between the brand name versus the generic drug name.
The danger of advising the untrained public to distribute emergency medicine
Many clinicians, let alone the general public, are not specifically trained in the proper dosage and treatment with Naloxone for the various forms and dosages of opioids and heroin.
FDA Advisory Committee on the Most Appropriate Dose or Doses of Naloxone to Reverse the Effects of Life-threatening Opioid Overdose ... Sept 2016
"The effectiveness of naloxone, and thus the exposure required, will depend on the opioid dose, the potency of the opioid in binding receptors, the lipophilicity of the opioid in crossing into the CNS system and the elimination half-life of the opioid, together with patient factors (7, 26). Appendix [2] and [2a] includes further information on naloxone pharmacology. The complex pharmacology of appropriate dosing is further compounded as often the fentanyl involved is illicitly manufactured without normal procedures or controls and may be introduced surreptitiously into heroin or prescription painkillers. Reports from the field confirm the need for additional naloxone doses to reverse opioid overdoses including those involving more potent fast onset synthetic opioids."
Narcan (Naloxone HCL) Use in Opiod Overdose: A Perspective
by Joan M. Rider-Becker, BS, PharmD, FMPA
Retired, Emeritus Professor, Pharmacy Practice Ferris State University College of Pharmacy Education/Training
B.S. Pharmacy-Ferris State University College of Pharmacy-1987
Pharmacy Practice Residency-Bronson Hospital Kalamazoo, MI-1987-1988
Doctor of Pharmacy (PharmD), University of Michigan-College of Pharmacy Ann Arbor, MI 1990
I have used opioids now for chronic pain management after a car accident almost twenty-years ago. I will admit, I was taken aback by my family physician about a month ago being given a prescription for Narcan (generic name Naloxone) as a “precautionary measure” for my chronic opioid use. The form I was prescribed is a nasal formulation vs. the oral/injection form. When I took it to a pharmacy to be filled, I had to undergo “special counseling” by a pharmacist (even with my credentials) which consisted of a video on proper use and a warning that after use, 911 had to be called and I was to be taken to the emergency room for follow-up. This is the proper follow-up when someone is prescribed any rescue medication for a drug reaction. The Naloxone is only to be given when a known opioid (i.e. codeine and it’s derivatives; Fentanyl, Meperidine, etc...) is given or taken in life-threatening incidences. I was instructed, "Were you aware that Naloxone has two elimination half-lives because this drug has an active metabolite; and, were you aware that Naloxone and Naltrexone are different agents, but are easily confused."
I believe giving someone this agent for overdose situations is giving a false sense of security that nothing else needs to be done. Nasal Naloxone is like putting a bandage on a cut artery. You may stop the blood flow at the moment, but the wound will continue to bleed if the wound isn’t sutured properly. Without appropriate emergency room follow up of an opioid overdose the person may die from that overdose.
Many opioids vary in dose, strength, predictability and most of all drug half-life. Knowing the half-life of drugs is essential to know how long the drug is going to last in your body. Drug half-life’s, drug absorption, distribution and elimination is well covered in Colleges of Pharmacy in courses such as pharmacology, pharmacokinetics and pharmacotherapeutics. Pharmacists do not know the pharmacokinetics on every drug substance out there by memory, and we are called the drug experts. Physicians do not have nearly as much education on medications as pharmacists, yet they are the first line of treating drug overdoses in emergency situations along with the nurses, Physician Assistants and Nurse Practitioners.
The general public is being provided a false sense of security by the media to carry this drug in their homes to address the opioid crisis. The public needs to be AWARE there is more to treating an opioid overdose than just squirting this agent up their nose.
| by Rose Rohloff | Another common practice over the past decade is the prescription of broad spectrum antibiotics for non-life threatening conditions. Broad spectrum antibiotics are for use in life threatening conditions/sepsis when there is no time to wait for a culture, or the inability to do a culture. Broad spectrum antibiotics target the necessary bacteria needed in the adult intestinal tracts; and so, the standard practice has become the second prescribing for probiotics; the requiring of multiple medications to be taken. Additionally, numerous reports over the last 10 years have shown the continued misuse of antibiotics (e.g. CDC Grand Rounds) causing antibiotic resistance, with the need for more and more antibiotics to be created and used. |
What has caused the layering of medications
Consumer engagement is needed with all medications being prescribed to be fully empowered, to understand: 1) the need for prescriptions, why and when appropriate, 2) the side effects of medications to determine alternatives versus adding on more medications, and 3) to eliminate the misuse of medications without the continued layering of additional drugs. Antibiotics should only be used when the body, given time, cannot fight a severe bacterial infection. And, antibiotics should only be given out after a culture is performed to eliminate a virus as the cause, or to target the specific bacteria. Broad spectrum antibiotics should only be used with life threatening-septic issues while waiting for a culture, or there is not the ability to perform a culture.
| Dr. Lee Beecher and David Racer in their book Passion for Patients wrote, "Dr. Kübler-Ross … called me to her office … “Ach, you’ve got a problem.” She said I needed to more clearly communicate... You have to learn about how to be a good son-of-a-bitch.” Pritzker (medical school at University of Chicago) taught me how to be a problem solver ... No one told me what I had to believe or how I had to think. They taught me how to think and apply what I learned to help my patients." (pages 55-57) Today I read someone describing the Forbes article by Brent Gleeson, “Apparently, during SEAL training, peer reviews are a weekly event. They have a process called top five, bottom five. Every week you anonymously rank the top five performers in the class as well as the bottom five.” Unfortunately, with political correctness and mandating diversity in healthcare, leaders and peers cannot or choose not to do ranking and hiring based upon performance. I have seen in the health industry that no one is allowed to hurt a doctor/nurse's feelings because they are being incompetent or under-performing, with patient's lives at stake. | It is a wonderful idea of ranking on performance so everyone pushes each other to excellence. But when a 30 year veteran nurse is told to shut up because she was holding accountable the new doctors and nurses not performing, competency rating (especially by knowledgeable veterans) was a great practice that worked 20-30 years ago - but one that is not tolerated today. The result, medical errors are now the #3 cause of death. The industry is killing people with our focus on kindness versus caring competency. Personally, I want a well trained, experienced, compassionate son-of-a-bitch taking care of me, as opposed to someone who is being nice while not knowing what they are doing. I want a doctor and nurse who takes care of me so I can go home and I don’t have to see them again because they are my quality clinicians, not my pals. |
Elisabeth Kübler-Ross, Passion for Patients, (page 62)
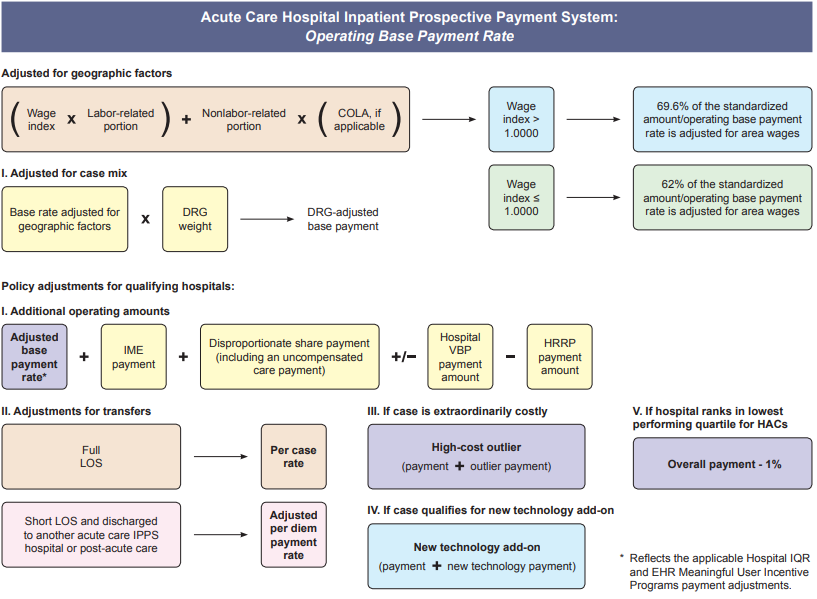
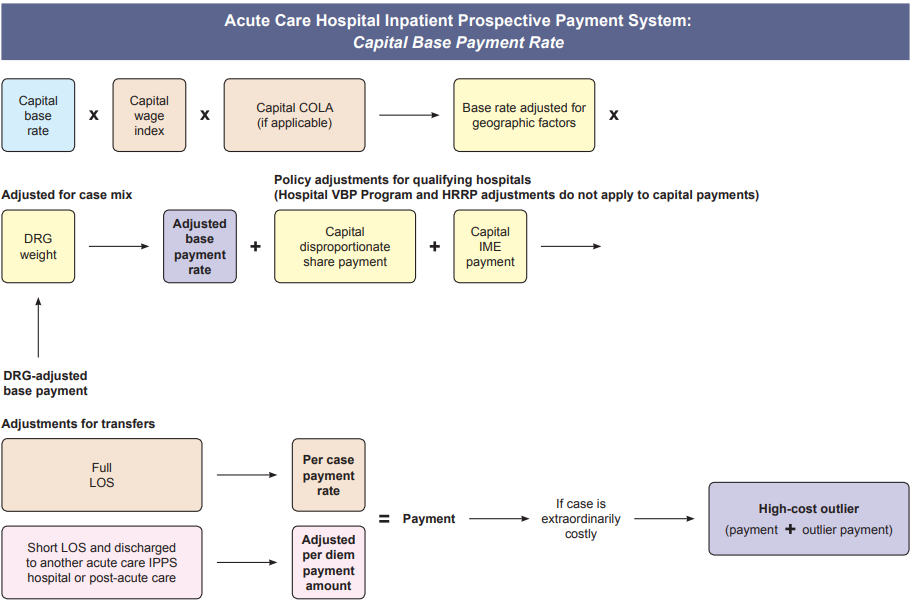
The media writes about the desire for transparency with many in the public demanding posted costs for healthcare; however, the public fails to understand - healthcare is not the same as other businesses. First, in business production & marketing creates increased sales volume. Whereas, in healthcare volume is driven by need, and the primary goal of providers should be getting, keeping people healthy, in effect driving away their business. Second, the highest percent of revenue for hospitals comes from the government agency Health and Human Services (HHS), especially the Medicare division. Below is the formula for calculating inpatient payment. So unlike businesses, utilities, or other services, healthcare costs, prices and payments are not simple amounts to readily comprehend. Healthcare information has been publicly available, now is the time to educate consumers in the population of how to find and understand it to champion their care.
Day’s statements exemplify an important component that has been lost in healthcare training - that of muscle, or specifically, movement memory. Clinicians are supposed to be trained in school regarding the need and proper technique for handwashing. More importantly, clinicians used to have extensive clinical time working in patient areas developing the movement memory for proper hand washing, and automatically keeping in mind what is clean vs. dirty, where established sterile fields are located with maintaining of sterile gloved hands. The training was extensive and repetitive, for clinicians to automatically move appropriately in fast paced, life threatening situations - to not have to think and just act. One common, simple example is the insertion of IVs for fluid administration or needles for drawing blood. The needle or IV cannula (the needle with covered sheath inserted into the vein) is sterile, with clinicians wearing nonsterile gloves. The skin is typically wiped with alcohol to clean, and then all too often clinicians press nonsterile gloved fingers on the cleaned skin to feel for the vein; thus, contaminating the cleaned surface of the patient’s skin where insertion directly into their vein will occur. Even though the nurse/doctor is wearing clean gloves, they are not sterile, and worn to protect the clinician. With repetitive movement training, clinicians would press to find the vein before properly cleaning the skin, and clean their gloved fingers at the same time as the patient’s skin.
Two frequent complaints often heard from patients, "They dug around in my arm and could not find the vein, it was so painful." "They poked me five times because they did not know what they were doing." Blood draws and starting IVs is a skill, just like shooting at a target or in high stress a gun fight, that requires proper training of technique, and more importantly, repetitive practice - especially with the understanding when someone's life depends upon it. Additionally, the conditioned good technique should be second nature to purge ALL air from needles and tubing, including from the side ports of IV tubing, to prevent the potentially fatal embolus as a hospital acquired condition (HAC).
With the great reduction of hands on clinical time in schools (with replacement of online theory, population/global health, writing, and shadowing nurses), this movement memory training has been lost, with the shift of cost to hospitals for training, buying expensive monitoring equipment, or addressing the subsequent HAIs/HACs. Bringing the ingrained, repetitive movement training back to school training would instill within clinicians and CNA/PCT caregivers the instinctual, reactionary awareness of dirty versus clean or sterile, and proper IV/needle insertion, while delivering care; whether normal daily care or imminent life versus death situations – because they just do what they are trained to do without having to stop and think through quality actions.
WatchPAT is an FDA-approved portable diagnostic device that uniquely uses finger based physiology and innovative technology to enable simple and accurate Obstructive Sleep Apnea (OSA) testing while avoiding the complexity and discomfort associated with traditional air-flow based systems.
by Rose M. RohloffMany articles and discussions have centered around the rise and demise of Theranos. The company valuation and strategy were based on their technology for running multiple tests, at reduced cost, utilizing a pin-prick instead of a regular needle blood draw. Learned lessons from the devaluation and closing of the labs and blood testing centers include the lack of transparency, the need for thoroughly vetting new innovation, the requirement to understand the actual market, the need to support vision with qualified proof-of-concept, as well as deficient oversight and due diligence - to name a few. One lesson of success, however, has been overlooked: The model of a needed paradigm was beginning to be established. Leaders in the healthcare industry tout the need for enabling consumers to be more engaged with their own health. The vision for Theranos to offer new blood testing technology also precipitated three (3) key factors supporting increased consumerism: | 1- having lab results sent simultaneously to consumers/customers at the same time to their physicians, within 24 hours; 2- the passage of AZ law HB 2645, enabling individuals to order their own blood tests from a licensed clinical lab without a doctor's order, paying cash; and 3- easier access to get lab tests performed through multiple, local health and wellness pharmacies, instead of going to a lab or hospital. This paradigm has not been discussed as successful, and one key component for involvement with control over one's own health, expanding the traditional care continuum to a health maintenance continuum. |
With the many lessons learned from an aborted (shady) startup, marketed to disrupt the healthcare industry with its counterfeit technology, the direction for having consumer-driven as the process should not be overlooked - and actually be revisited to expand upon the great health ownership model of good disruption to healthcare.
Ms. Rohloff, a 35-year healthcare veteran with experience in nursing, business and information systems, spoke with Becker's Hospital Review about providing consumers with more detailed evaluation of quality care delivery. [read more]
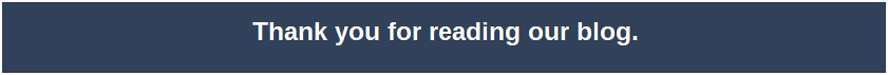
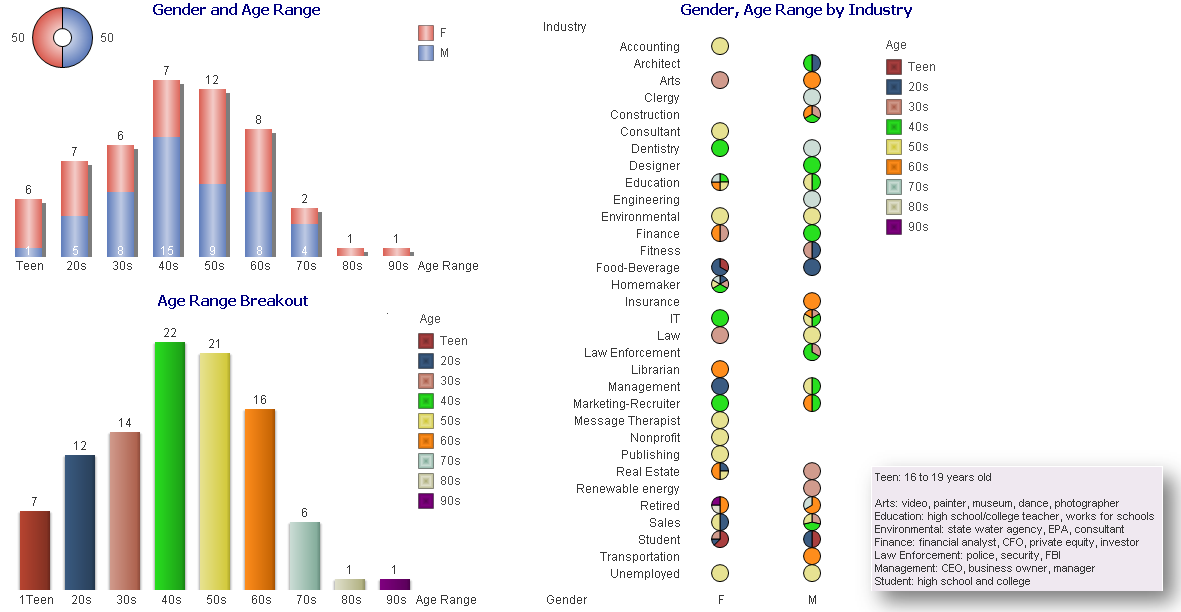
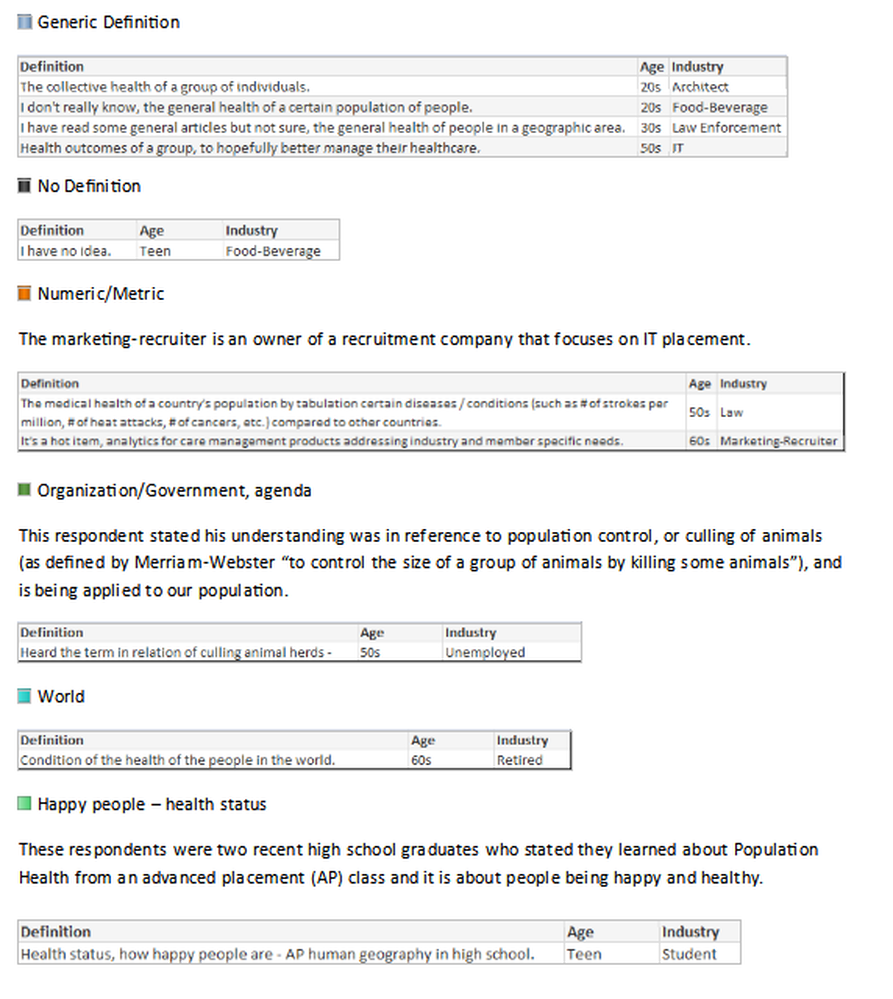
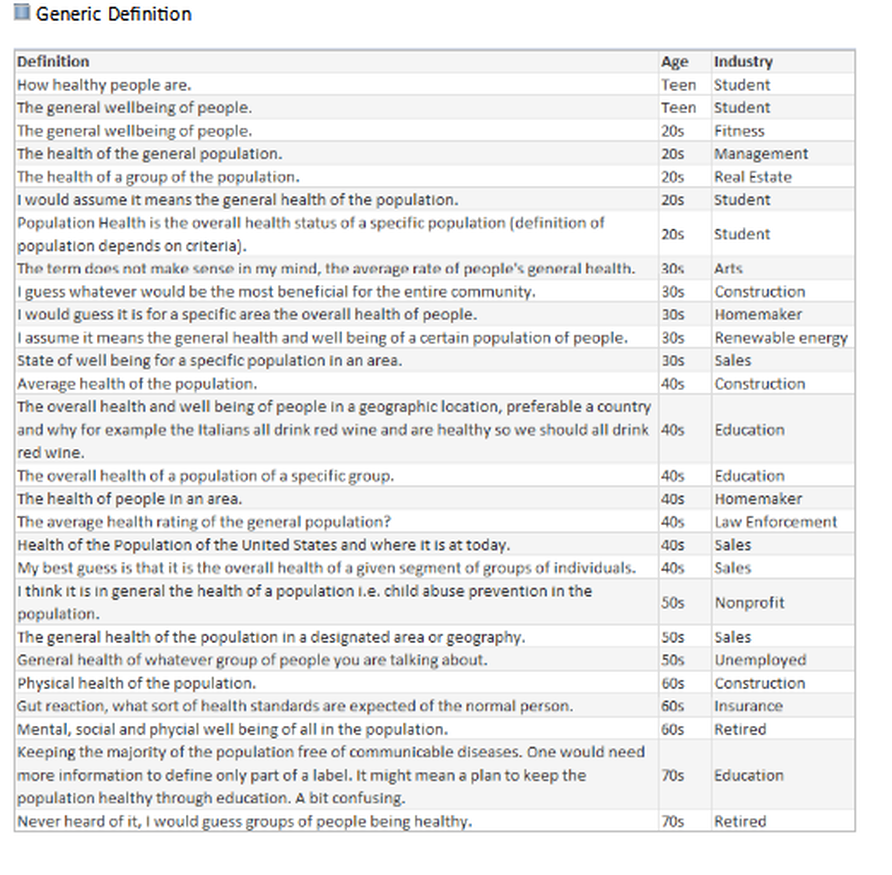
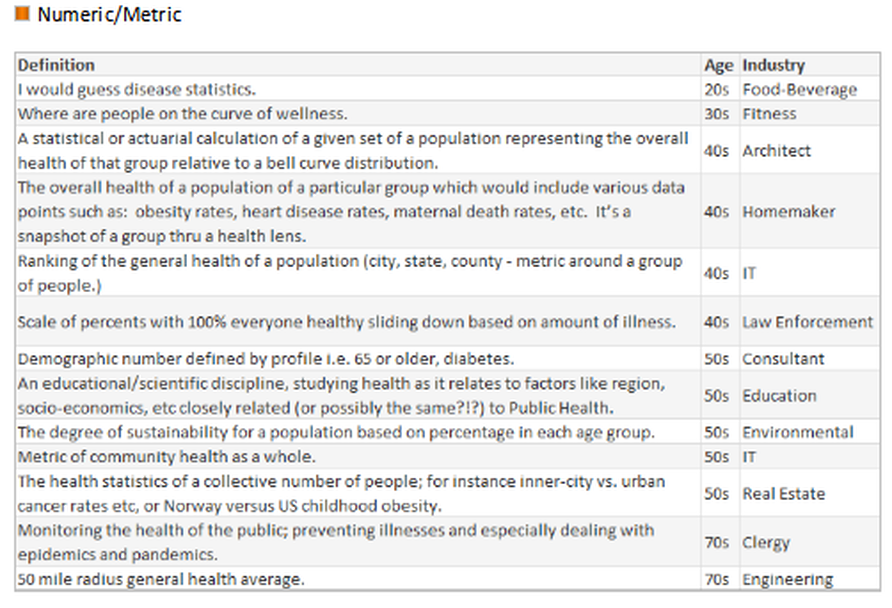
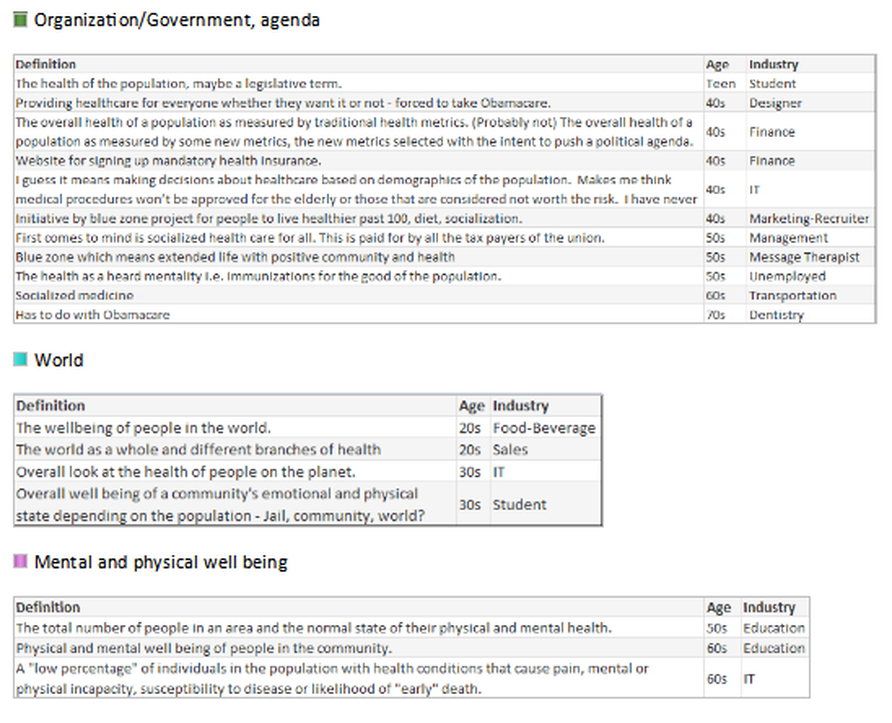
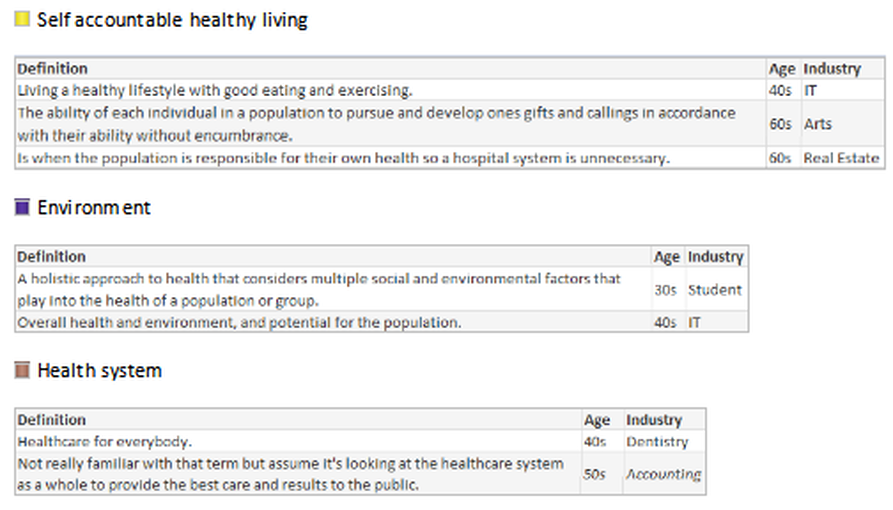
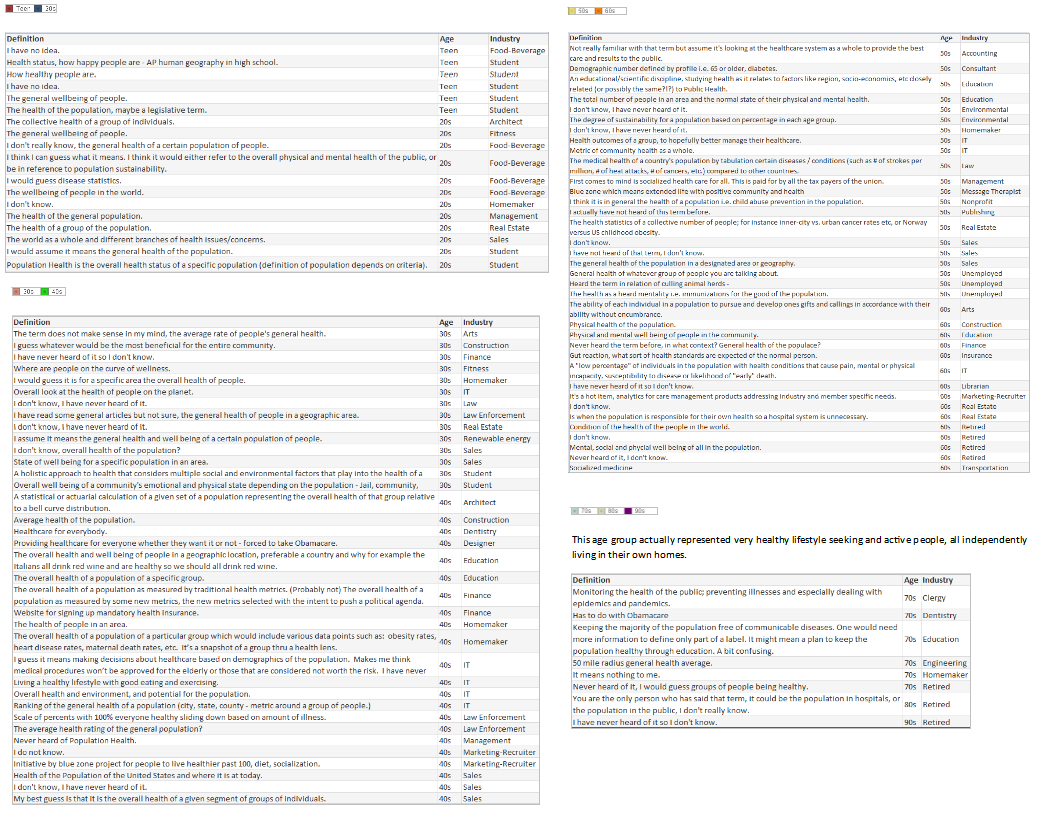
Lacking a uniform definition makes it difficult to define when healthcare has succeeded, to establish key performance indicators (KPIs) for monitoring progress, to determine which solutions lead to that success, and most important to educate the population on what initiatives and goals are being offered to help them. After performing the industry survey, I thought about one important step healthcare leaders have not done - ask the consumer, those individuals who make up the population - what is the public’s understanding or desire for Population Health.
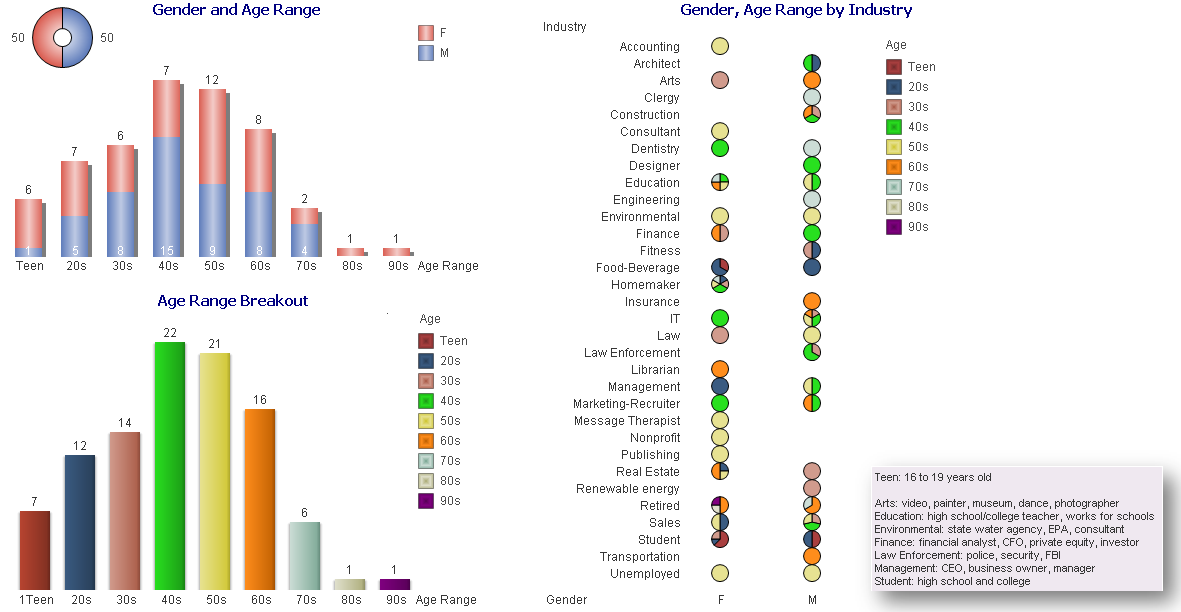
With this in mind, I wanted to conduct a survey of 100 non-healthcare people across the country, of various ages, a range of industries, and regardless of political affiliation. Each person was asked:
- Have you heard the term Population Health before? Yes/No
- What does Population Health mean?
Many people looked confused upon being asked those questions and stated they have never heard the term before, while others provided an immediate description. Although the survey showed the lack of any definitive definition, and verified the general lack of understanding of the concept, it showed how much the public wanted to talk about Population Health, with several people engaging me in conversation to find out what the industry is doing and asking, “What is the actual definition?” *https://www.hfma.org/BIgoals/
Survey Results
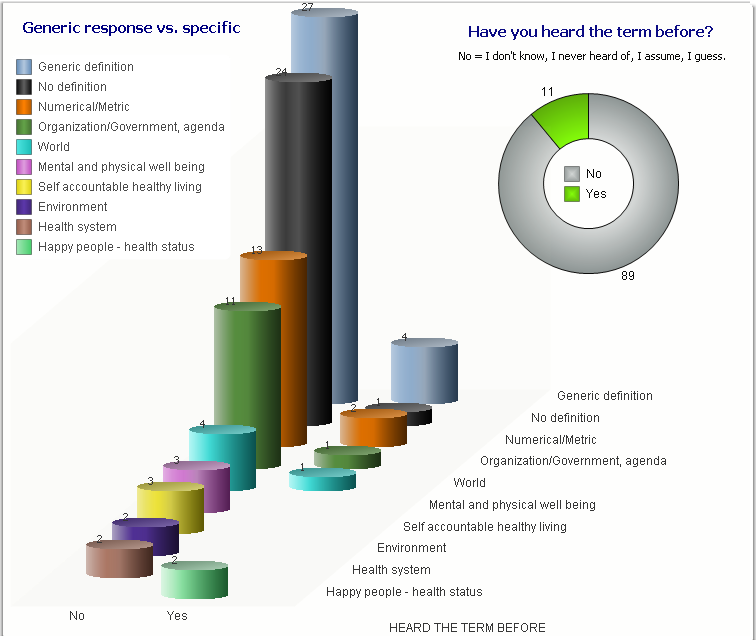
What is your understanding of the definition?
- Numeric: The marketing-recruiter is an owner of a recruitment company that focuses on IT placement.
- Organization/Government, agenda: This respondent stated his understanding was in reference to population control, or culling of animals (as defined by Merriam-Webster “to control the size of a group of animals by killing some animals”), and is being applied to our population.
- Happy people – health status: These respondents were two recent high school graduates who stated they learned about Population Health from an advanced placement (AP) class and it is about people being happy and healthy.
In the hfm article, I proposed that the industry standard definition needs to include “a partnership with the community of health seeking persons” including “putting data into the hands of patients and encouraging them to share accountability for health outcomes by choosing healthy lifestyles, following health regimens, and seeking health education.” As the public survey shows, we in the industry need to ascertain their understanding, and have a collaborative relationship for population health management with a clear definition and public education regarding solution offerings.
What would be your understanding of a definition?
As a general finding, respondents between the ages of:
16-17 Wanted to convey input.
18-20 Had general apathy regarding the topic and generic input without additional inquiry.
30-40 Showed the highest desire to participate and have conversation regarding – the largest group with children and facing older parents with increased health concerns.
50-60 Wished to participate with continued conversation regarding what is happening in the industry with more defined ideas of what the term means.
70-90 Were an active and health conscious group being very productive in their communities and had a desire to learn about the topic.
Summary
| The bottom line of my hfm article and this survey, healthcare loves to create ambiguous terms and focus spending on generalities without quantifiable results, and focused on the masses - not on individuals. There is a quote attributed to Sam Walton, “There is only one boss, the customer. And he can fire everybody in the company from the chairman on down, simply by spending his money somewhere else.” While performing inquiries of the public, I have spoken to many people who shared the desire to control their own health decisions along with integration of standard and holistic medicine, and unfortunately several who are currently seeking health care in other countries. | A veteran health care consultant and nurse summarized this by responding: I read your recent article in HFMA Defining BI Goals for Coordinated Care and Population Health. You are spot on with the questions and approach the healthcare community should take, but do not, with population health strategies. It will not be surprising to see how many resources are used by healthcare systems and providers in their attempt to ‘manage their population’s health’ while the population continues to choose which provider (s) to receive care from during sickness and health. Until 2017 and 2020 when the FFS reimbursement model begins to shift, I suspect we will see outcome changes in larger healthcare systems that are engaged in an ACO and HMO model, but not significant enough across all healthcare systems. |
Addendum: all answers by age groupings
click an article
to read and post comments
Search topic
select category
All
APAC Teams
Care Quality
Champion Your Own Care
Clinician Quality Education
Experience Satisfaction
Healthcare Consumerism
Health Innovation
Medical Care Coordination
Palliative Care
Patient Engagement
Physicians
Population Health
Transitioning Care Coverage
search by date
July 2024
June 2024
April 2024
March 2024
February 2024
January 2024
November 2023
October 2023
June 2023
May 2023
October 2022
September 2022
July 2022
August 2020
April 2020
January 2020
June 2019
May 2019
April 2019
October 2018
September 2018
August 2018
July 2018
May 2018
April 2018
March 2018
February 2018
January 2018
December 2017
September 2017
June 2017
October 2016
September 2016
May 2016
March 2016
October 2015
June 2015