Compiled Rose Rohloff from input by Dr. Peter McCullough and Dr. James ThorpMany persons may have been illegally coerced into taking the Covid shots.(see blog entry regarding the 1974 National Research Act) The following is an extensive Spike Protein (SP-C) lab panel, sectioned into subpanels (a panel is a collection of several lab tests), for evaluating if you systems may have been impacted by the spike proteins - with or without existing symptoms. Note some individual labs may be duplicated in various panels and will not have to be duplicated. Champion your own care and consult with your choice of physician with informed consent. General Tests and Evaluation of Cardiac
The following evaluate antibody (Ab) in your blood, proteins made by the immune system to fight foreign bodies (bacteria, virus …)]**
For women of reproduction age
For autoimmune and/or bleeding issues
1No commercially available test for circulating spike amounts are available at this time and will update as one becomes available. Serum Spike Antibody (Ab) is the surrogate at this time. Higher spike Ab titer correlates with severity of infection/long COVID. Pathologists are able to determine if tissue spike is from Shots/Injections versus infection via correctly performed autopsy, as per Dr. Ryan Cole in deposition of case. “Normal” Value-ranges & Description of various testsSome parameters vary slightly based on which lab is used - low or high readings should be determined by the specific lab being used at the time of lab test, and for individuals regarding their baselines, underlying conditions. D-dimer CBC CRP CMP Various Antibody testing to determine if your immune system is or is not fighting off a foreign substance. TSH: ***
Amenorrhoea Panel
0 Comments
by Rose RohloffMore than ever in today’s healthcare, it is imperative for consumers to champion care themselves or have someone act as their health care champion. People are not experts in disease management and need to know what questions to ask. Individuals will not fully process information while in a compromised emotional state (some refer to only 20% of information being heard and comprehended while under duress) – as the following story demonstrates. A wonderful, young mother of small children contacted me and relayed her experience. She had gone into remission from a potentially life-threatening condition. After eight years of being asymptomatic while off all drugs, she began to experience the onset of new symptoms. With a recent scan performed, she went to a new doctor in her small town to get the scan results, I refer to him as Dr. A. Dr. A looked at me and asked, “Why are you crying? You knew that you have Multiple Sclerosis since you were in your 20s.” Dr. A did not consider that his patient was now a mother of small children, and her primary concern is always how to care for them - the situation was no longer about herself; she was sitting in front of him alone; and, she now lives in a small town without access to an expert in her disease management. The doctor did not recognize that his patient was thrown off balance by his comment, and she was not comprehending what was being said.
A Healthcare Champion is Always Needed |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| I coined the term health care champion instead of advocate because advocacy has morphed to represent gaining access to doctors and payment/reimbursement. Advocacy is steering to a directory. A champion is a person or team beside you to guide, interpret, do leg work for understanding, monitor for quality, and in many cases fight for you! |
- the "shotgun" approach of running pages of tests hoping to hit something;
- symptom = prescription, take a symptom and throw a drug at it;
- failing to do comprehensive H&Ps, assessments, and clinical diagnosing.
A Partnership Always Needs to Exist for Quality Care
Population health is an established community of people (consumers), working in partnership with health providers, advocates and educators operating holistically as a team within an integrated health maintenance continuum, to perpetually achieve and enhance quantifiably agreed-upon quality of life outcomes.
A career physician told me years ago, "Being a doctor used to be a calling: Today, many physicians see it as just a job, without a desire to put in the hours and work often needed establishing a rapport with patients."The previous story I shared, about a young mother addressing the news of the possible relapse of a disease, demonstrated the importance of having a healthcare champion.
I read the June 2017 article in BECKER’S Hospital Review, “Younger physicians may have less faith in the Hippocratic Oath, which has a patient focus, because they feel it no longer holds in today's healthcare environment in which many needs compete for their attention.”
The notion that the oath or code of ethics, being patient focused, does not hold in today’s healthcare is poignant because … “there is art to medicine as well as science, and that warmth, sympathy, and understanding may outweigh the surgeon's knife or the chemist's drug.”*
*The modern version of the Hippocratic Oath was written in 1964 by Louis Lasagna, Dean of the School of Medicine at Tufts University. [Similarly, the AMA Medical Code of Ethics.]
Realistically, physicians are pulled in multiple directions, and in many cases overloaded with people requesting to be seen: This does not mean that physicians should lose sight of how to respond with patients, keeping them the focus, nor should reimbursement needs and learning electronic medical records supersede the patient. It does mean with more volume demands, physicians need to rely on a team approach for providing comprehensive communication, alignment with patient’s understanding of things and their wishes, along with realizing that oaths and the code of ethics hold clinicians to a higher standard. The team approach is necessary for quality care and caring, including the person being cared for and their champions.
9th Circuit Court Ruling |
(1) The court ruled that the district court misapplied the 1905 Jacobson case because LAUSD relies on a drug that Plaintiffs plausibly alleged did not prevent the spread of the virus.
(2) LAUSD has changed its mind about requiring the vaccine and therefore, the case cannot be mooted because LAUSD has proven it will just enact it again later.
(3) The court said, "But even if the materials offered by LAUSD are subject to judicial notice, they do not support rejecting Plaintiffs’ allegations. LAUSD only provides a CDC publication that says “COVID-19 vaccines are safe and effective.” But safe and effective for what? LAUSD implies that it is for preventing transmission of COVID-19 but does not adduce judicially noticeable facts that prove this."
(4) "Pursuant to more recent Supreme Court authority, compulsory treatment for the health benefit of the person treated—as opposed to compulsory treatment for the health benefit of others— implicates the fundamental right to refuse medical treatment. Plaintiffs’ allegations here are sufficient to invoke that fundamental right. Defendants note that the vaccination mandate was imposed merely as a “condition of employment,” but that does not suffice to justify the district court’s application of rational-basis scrutiny."
(5) MUST READ THIS..."In Washington v. Glucksberg, 521 U.S. 702 (1997), the Court explained that Cruzan’s posited “‘right of a competent individual to refuse medical treatment’” was “entirely consistent with this Nation’s history and constitutional traditions,” in light of “the common-law rule that forced medication was a battery, and the long legal tradition protecting the decision to refuse unwanted medical treatment.” Id. at 724–25 (citation omitted). Given these statements in Glucksberg, the right described there satisfies the history-based standards that the Court applies for recognizing “fundamental rights that are not mentioned anywhere in the Constitution.” Dobbs v. Jackson Women’s Health Org., 597 U.S. 215, 237–38 (2022). The Supreme Court’s caselaw thus clarifies that compulsory treatment for the health benefit of the person treated—as opposed to compulsory treatment for the health benefit of others— implicates the fundamental right to refuse medical treatment." https://cdn.ca9.uscourts.gov/datastore/opinions/2024/06/07/22-55908.pdf…
by Rose Rohloff
THE ORIGINAL HIPPOCRATIC OATH ALTERED & EXPANDED
I (name) will perform my duties with faith and trust in God as my guide, and continually learn as long as I perform my duties. I will impart a knowledge of the art of healing, mentoring and teaching those I serve. Above all else, I will abstain from whatever is deleterious, mischievous, malfeasance or unjust to those being treated, and I will not break what is not broken, for that is doing harm.
I will use those dietary regimens which will benefit the persons I see, according to my greatest ability and judgment, always providing proper informed consent of all alternatives, ramifications, risks and possible outcomes - for any and all treatments, herbs, supplements, medicines, procedures and surgeries.
I will preserve the unalienable rights endowed by the Creator on every individual human life, from conception to natural death. I will not give a lethal drug to anyone if I am asked, nor will I advise such a plan for intentionally ending a life; and similarly I will not give a woman or cause an abortion. In purity and according to divine law will I carry out my life and my art. I will enter them for the benefit of the sick, avoiding any voluntary act of impropriety or corruption, including the seduction of women or men. Whatever I see or hear in the lives of those I care for, whether in connection with my professional practice or not, I will keep secret, as considering all such things to be private.
I will, remain faithful to this oath and fiercely and honorably battle illnesses regardless of societal coercion, derision by others or imperilment to my livelihood and life. So long as I maintain this Oath faithfully and without corruption, may it be granted to me to partake of life fully, and the practice of my art to heal and mentor for staying healthy, giving glory to God for His gift of healing. However, should I transgress this Oath and violate it, may the opposite be my fate.
So help me GOD.
they abide by, adhere to, and practice within its ethos?
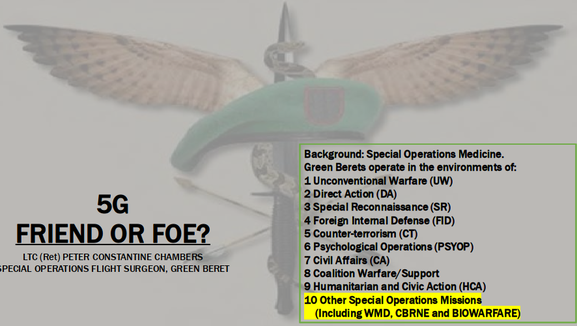
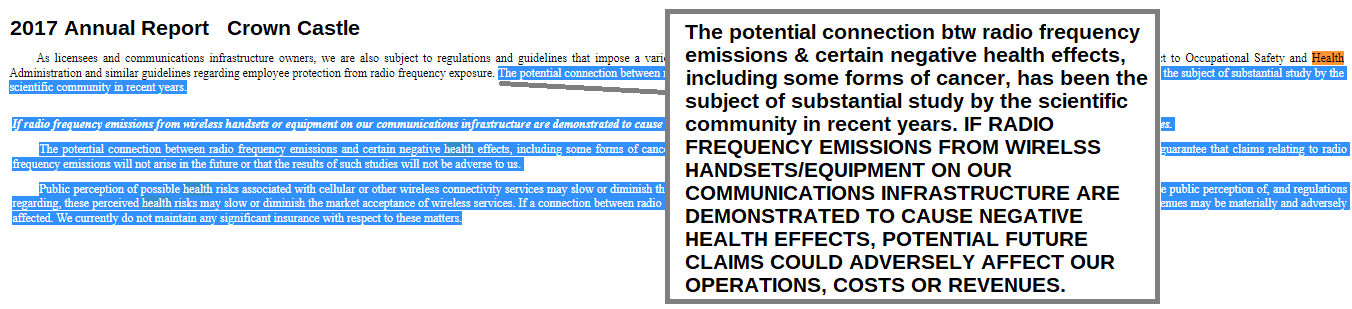
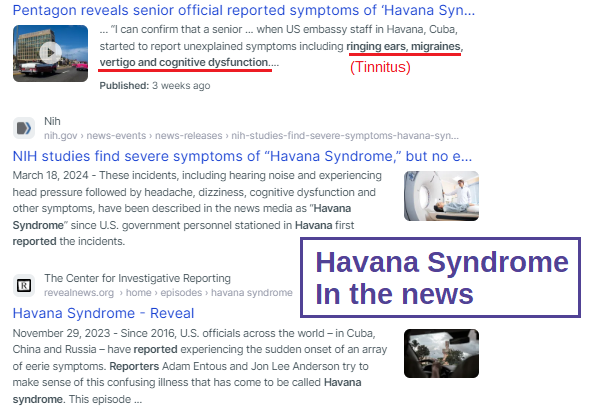
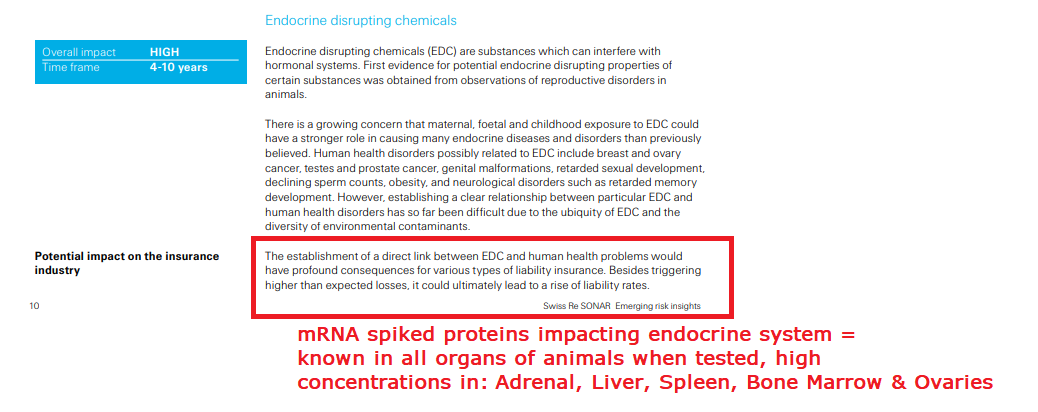
Who is in charge of healthcare? Is your Health insurance coverage invalidated/exempt? 5G and edc
4/12/2024
by Rose Rohloff
Laws and Executive Orders (EOs) regarding healthcare under "public health"
Open "disease" cart blanc for them to choose (or orchestrate?)
March 2, 2023 "Although the accord is being called ... a treaty or another kind of binding agreement, such as the WHO Framework Convention on Tobacco Control, or a nonbinding agreement, such as the Paris Climate Accord. “As with all international instruments, any accord, if and when agreed, would be determined by governments themselves, who would take any action while considering their own national laws and regulations,” a WHO spokesperson told us." Federal and Local Governments would be in charge regarding any Rights violations. The accord is accumulation of monies $$$ to be "distributed" to various countries/persons, in the name of public health.
| James Roguski - researcher, author, natural health proponent and an activist. In March 2022, James uncovered documents regarding proposed amendments to the International Health Regulations (IHRs), and was instrumental in raising awareness about them. James now works to expose the WHO's hidden agenda with ongoing attempts to amend the IHRs. | Let’s get out of the WHO author questions at 1:45:46 |
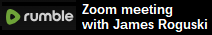
LTC (ret) Green Beret, Doc Pete Chambers, MD, bioweapons expert
| 5 G overview & Operation Crimson Mist
| |||||||||||||
of policies, being invalidated without the knowledge of people,
and against their choice - through lack of knowledge,
lack of informed consent, and through illegal coercion?
Electromagnetic Radiation
Endocrine Disrupting Chemicals (EDCs)
by Numerous experts
My desire is to provide several articles from those adroit in the subject. COPPER: the less talked about, and important trace mineral, the importance of Zinc, and when taking high Zinc, make sure you know the ratio of zinc to copper supplements.
"Excessive zinc supplementation can lead to a copper deficiency. That is because these two nutrients compete for absorption sites, and zinc preferentially binds for absorption." |
Ron Reece @Mujhunter | God's creation of finely tuned 'orchestra'Linus Pauling Institute ZINC: "Taking large quantities of zinc (50 mg/day or more) over a period of weeks can interfere with copper bioavailability. High intake of zinc induces the intestinal synthesis of a copper-binding protein called metallothionein (see the article on Copper). Metallothionein traps copper within intestinal cells and prevents its systemic absorption (see Wilson’s disease).
|
| Harvard Public Health "... (Copper) assist(s) various enzymes that produce energy for the body, break down and absorb iron, and build red blood cells, collagen, connective tissue, and brain neurotransmitters. Copper also supports normal brain development and immune functions, and is a component of superoxide dismutase, an antioxidant enzyme that dismantles harmful oxygen “free radicals.” Copper is absorbed in the small intestine and found mainly in bones and muscle tissue." | Liver Oysters Spirulina Shiitake Mushrooms Nuts and Seeds Green Leafy Dark Chocolate (Cocoa) NOT sweetened Salmon |
| "Researchers found that copper-based alloy surfaces have the ability to destroy a wide range of microbes and bacteria relatively rapidly - often within two hours or less. Several studies found that if touch surfaces are made with copper-based alloys, the reduced transmission of disease-causing bacteria can reduce patient infections in hospitals by as much as 58%." |
Professor Bill Keevil, head of the microbiology group at Southampton University, added his voice to the growing scientific consensus behind this by advocating the use of Copper and Brass door furniture, fixtures and fittings in public places and on public transport, as they could dramatically cut the threat posed by superbugs.
In research published in the journal Molecular Genetics of Bacteria Professor Keevil wrote: “There are a lot of bugs on our hands that we are spreading around by touching surfaces. In a public building or mass transport, surfaces cannot be cleaned for long periods of time… Until relatively recently brass was a relatively commonly used surface. On stainless steel surfaces these bacteria can survive for weeks, but on copper surfaces they die within minutes… We live in this new world of stainless steel and plastic, but perhaps we should go back to using brass more instead.”
In addition to direct contact killing of bacteria and harmful microbes, amazingly Copper surfaces have been found to exude an antimicrobial 'halo' effect on surrounding non-copper surfaces. Research in the intensive care unit a Hospital in Greece found that other surfaces up to 50 centimetres from copper surfaces experienced 70% microbial reduction, compared to the same surfaces with no proximity to copper-based materials. The ‘Halo’ effect was also observed in trials at a U.S. clinic in 2010. This amazing effect demonstrates just how powerful copper is as a weapon against bacteria." www.morehandles.co.uk
Videos to listen to
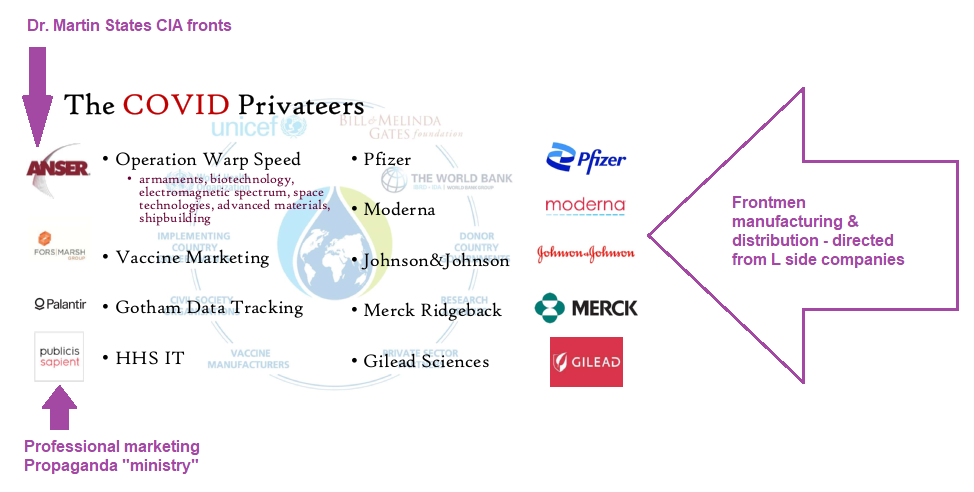
The latest simple, easy-to-follow overview of the paper trail showing crimes against humanity, and how a few of the many are now complicit with failure to act on the crimes,
The Great Setup, Part 1:
https://twitter.com/uimedianetwork/status/1756512994429735151?s=19
The Great Setup, Part 2:
https://www.uimedianetwork.com/294633/the-great-setup-part2.htm
Coronavirus Gain-of-Function Research at the Covid Summit in Brussels, Belgium May 2023
https://rumble.com/v2mwrgm--dr.-david-martin-documenting-coronavirus-gain-of-function-research-at-the-.html
Dr. Martin is impressive with his work, and how he articulates things https://twitter.com/i/status/1615707500946546689
Martin was the first to stipulate Pharma with DoD, CIA
7-12 minutes great breakdown of science that it is not about virus, protein fragment! 13 minutes Insert mRNA fragment, so cell makes Spike Protein.
17 minutes Acts of Terror
18 minutes AntiTrust laws violated, conspiracy
20 minutes Interlocking Directorates, Sherman Act
22 minutes Civil law, used by Trade Commission - cannot do deceptive marketing
27 minutes unlawful lack of informed consent Institutional Review Board never created, even in the case of emergency Code 21CFR section 50.24
by Rose Rohloff
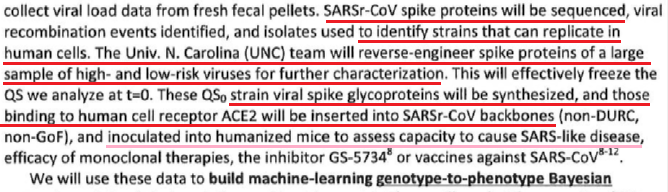
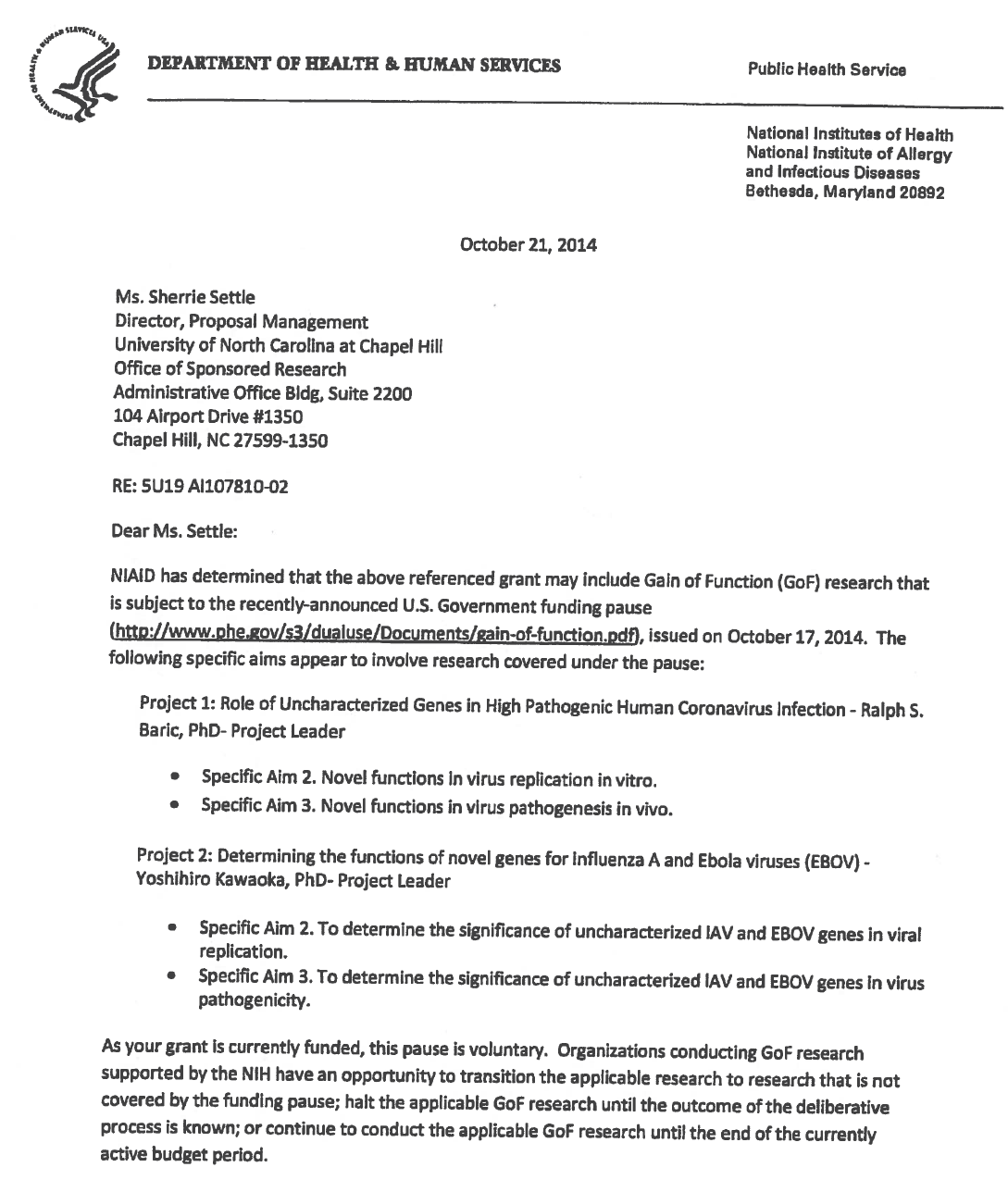
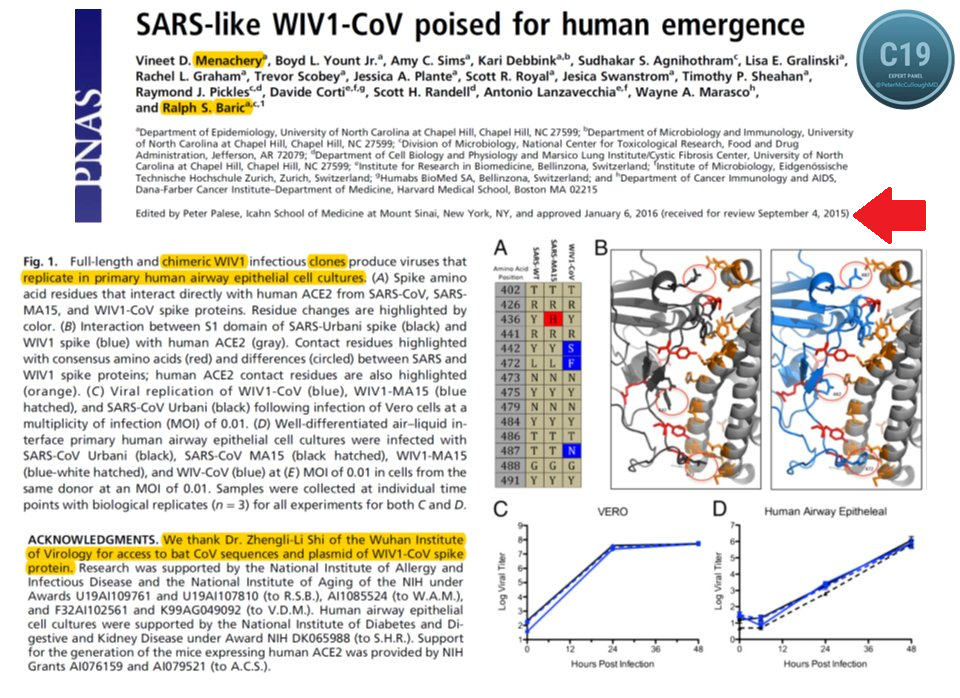
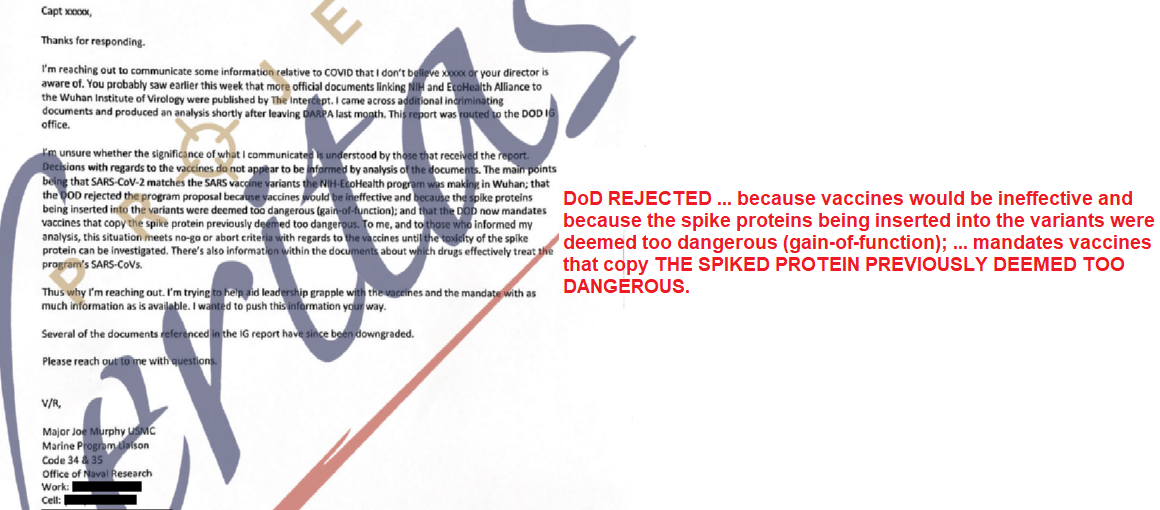
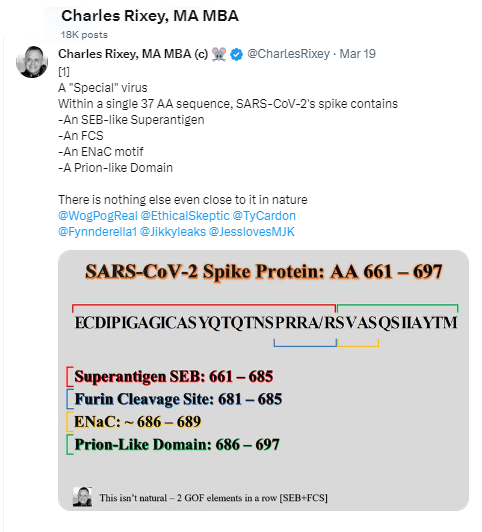
- EcoHealth Alliance (EHA) proposed to DARPA with intentional design
- DARPA refused because gain-of-function (GOF)
- EHA did anyways under the Health & Human Services (HHS-NIAID)
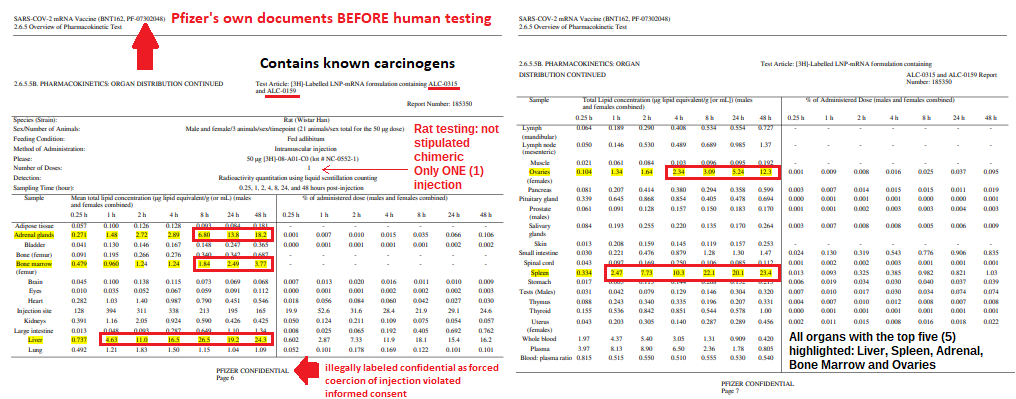
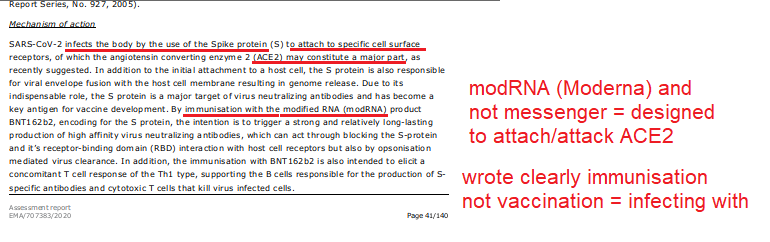
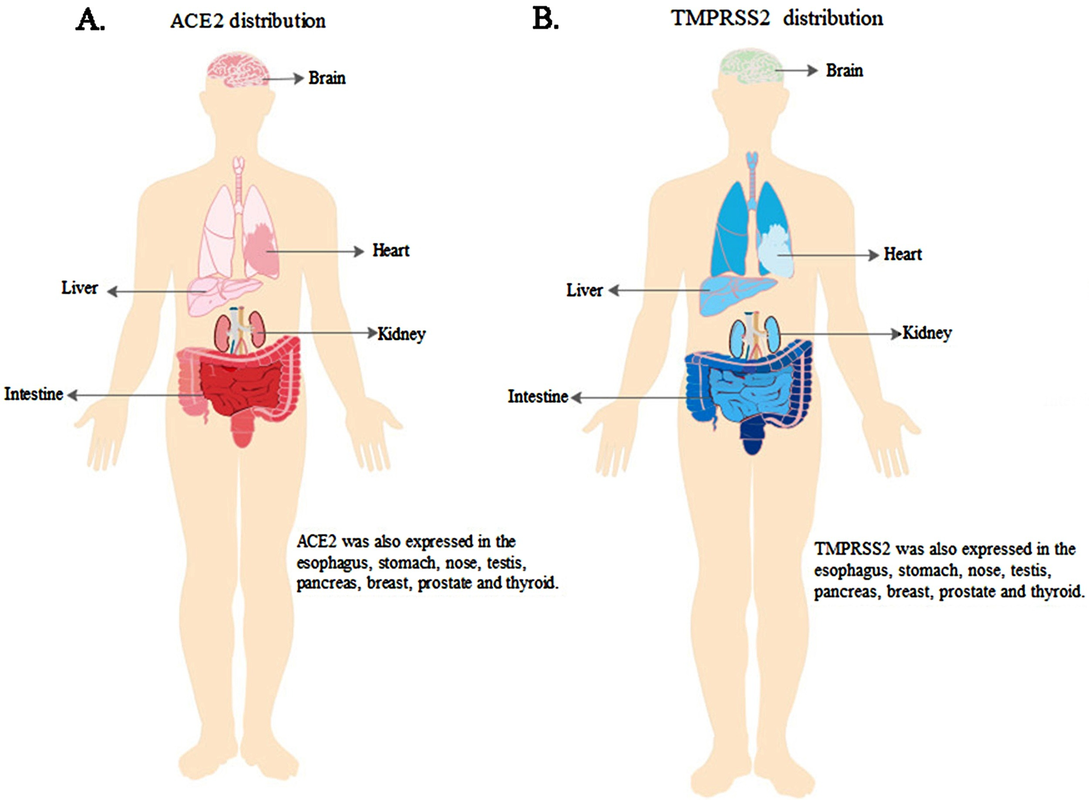
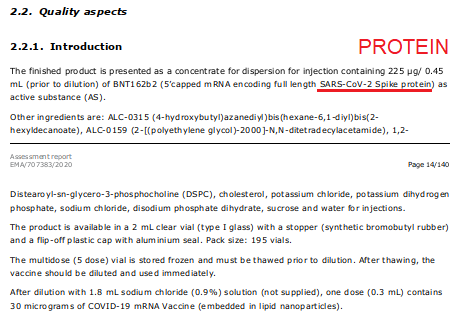
- The shots contain ACE2 binders - spike proteins
- Fauci at NIAID knew it was GOF
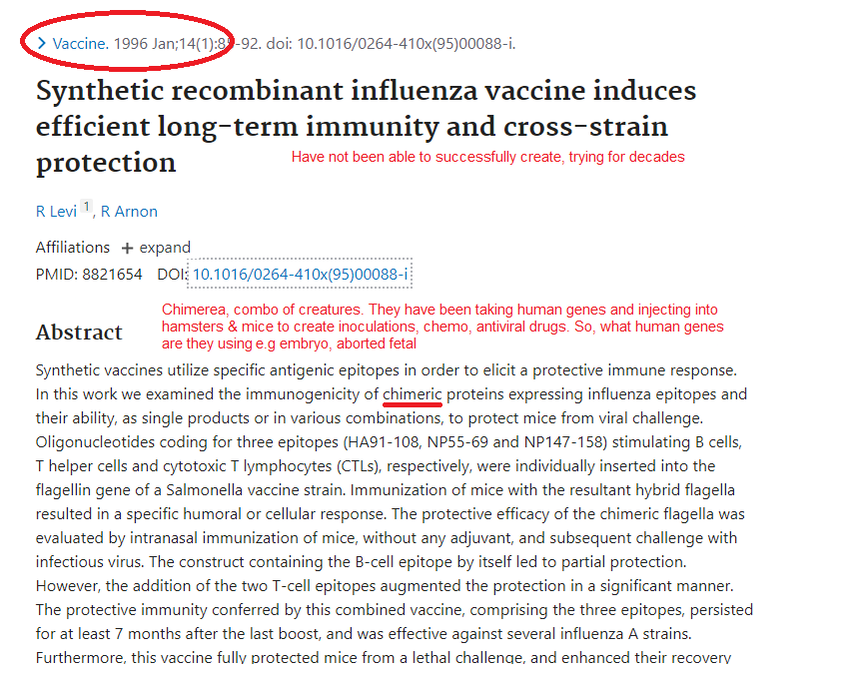
* Not natural: chimeric infectious clones, GOF
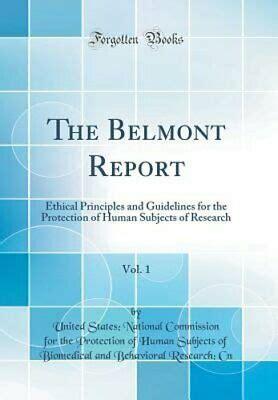
by Rose RohloffOn July 12, 1974, the National Research Act (Pub. L. 93-348) was signed into law, there-by creating the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. One of the charges to the Commission was to identify the basic ethical principles that should underlie the conduct of biomedical and behavioral research involving human subjects. |
- Dr. Hideyo Noguchi of the Rockefeller Institute for Medicine in Manhattan, New York City injected 146 hospital patients (some were children) with a syphilis extract (1911);
- Dichlorodiphenyltrichloroethane (DDT) wide use (1940s-1972);
- Nuremberg War Tribunals (1947);
- U.S. Navy sprayed large quantities of the bacteria serratia marcescens over the city of San Francisco, as part of Operation Sea-Spray (1950s);
- Mentally disabled children at the Willowbrook State School in Staten Island, New York, were intentionally infected with viral hepatitis, for research purposes, to help "discover a vaccine" (1950s - 1972);
- Thalidomide with massive birth defects (1950s-60s) which led to the Kefauver Amendment (1962) "... to the Food, Drugs, and Cosmetic Act, also known as the Drug Efficacy Amendments of 1962, was signed by President John F. Kennedy and requires that all new drug applications demonstrate substantial evidence of the drug’s efficacy for the marketed indication, in addition to the existing requirement of demonstrating the drug’s safety ... In addition, the Amendment required drug advertising to disclose accurate information about side effects and efficacy of treatments.;
- Lysergic Acid Diethylamide (LSD) experiments (1950s-60s);
- the Radiation experiments (injection of radioactive elements, including polonium, plutonium, and uranium, into civilian patients around the country, (April 1945 and July 1947);
- Tuskegee Syphilis Experiment (1930s-70s);
- Declaration of Helsinki in 1964 (updated 2000) built upon the Nuremberg code as the basis for Good Clinical Practices;
- Chester M. Southam, MD, a noted immunologist at Sloan-Kettering Institute, obtained funding from the government and injected live cancer cells into 14 patients with advanced cancer and into healthy convicts at Ohio State Prison, and injected live cancer cells into 22 elderly patients at Jewish Chronic Disease Hospital in Brooklyn (1954-1963) “Every human being has an inalienable right to determine what shall be done with his own body. These patients then had a right to know the contents of the syringe: and if this knowledge was to cause fear and anxiety or make them frightened, they had a right to be fearful and frightened and thus say NO to the experiment. (Oxford Textbook of Clinical Research Ethics, 2008)”
- Operation Crimson Mist, Rwanda (1994) electromagnetic augmentation (5G)?; now,
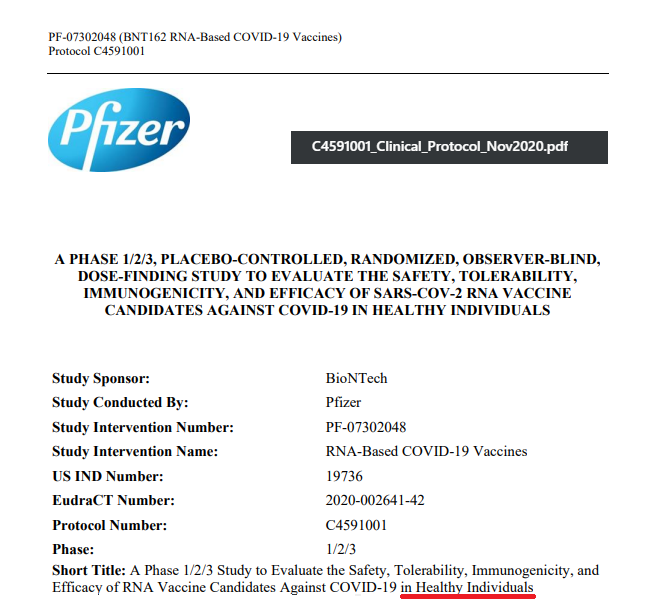
- Gain-of-function spike proteins, with mRNA/mmRNA/modRNA/Viral Vectors injections, does not fall under any legal definition of vaccine, with gross morbidity and mortality (2019 - ...)
| The law may not be negated, overwritten, or manipulated to force participation in experiments - by the government, employers, or companies, especially pharmaceutical companies - for whom the law was written to protect us; especially by labeling Emergency Use (EU). EU is for emergency circumstances with Informed Consent as part of Right to Try, if there are no other options for a patient. EU cannot supersede or try to negate the law especially regarding being fully informed with the Right To Say No - and the Right to Try alternative treatments.
| |||||||
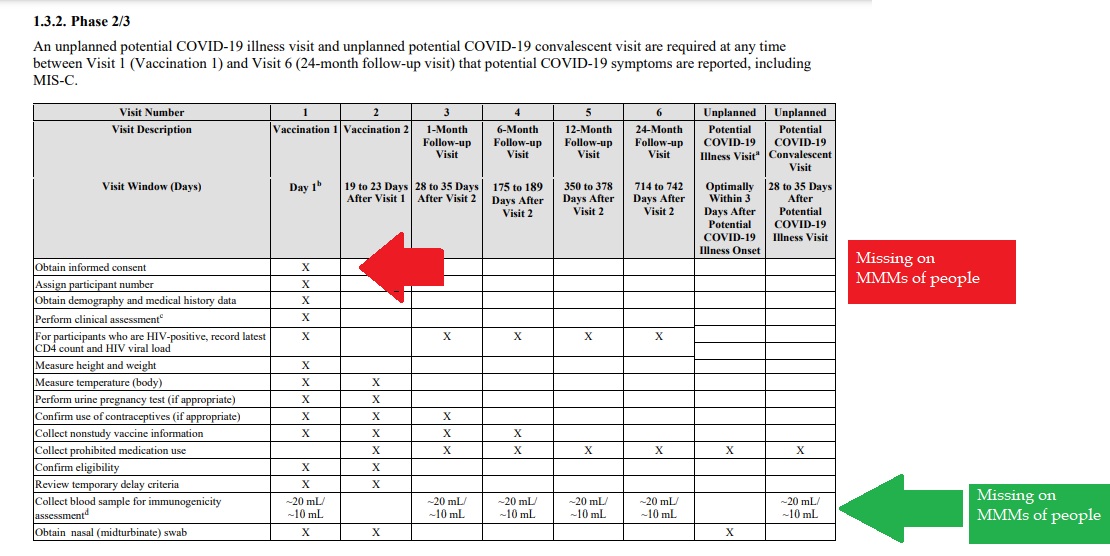
1- Autonomous agents, individuals capable of deliberation about personal goals and of acting under the direction of such deliberation. The Government and companies have to give weight to autonomous persons' considered opinions and choices, and cannot obstruct their actions and judgments, nor deny individual freedom to act on considered judgments, and cannot withhold information necessary to make a considered judgment. Necessary information includes - but not limited to - all medical opinions by established, industry experts, health status, the necessary assessments, labs, with close monitoring of physical lab and test follow ups of each and every autonomous persons as part of clinical research and testing, along with full documentation of testing, efficacy, use of chimera for research and testing, any and all conceivable side effects, and interactions of conditions.
2- persons with diminished autonomy are entitled to added protections.
Violators to the law have been marketing to the most vulnerable, including the immature and the incapacitated who were in need of extra, added protections, even to the point of excluding them from any injections or procedures which may harm them; violating added safety precautions for children, elderly, or those with diminished capacity.
Informed consent - must include full disclosure of ALL contents to be injected, any and ALL possible side effects (which can be several pages long), how those persons are individually to be closely monitored, safety guidelines, and above all the right to say no before or at any time, and full reporting of all individuals regarding their safety monitoring/labs/assessments, and any and all side effects. By promoting COVID shots all still under clinical trial/research, and coercing with careers/jobs, inability to travel, etc. in order to take the shots, this law is being violated through: lack of informed consent, lack of protections of autonomous persons, and/or illegally acting as IRB safety board members marketing to those not autonomous and capable of self-determination, with higher standards of protection to be invoked, and assuming the role for their safety.
The maxim "do no harm" has long been a fundamental principle of medical ethics. Claude Bernard extended it to the realm of research, saying that one should not injure one person regardless of the benefits that might come to others.
An agreement to participate in research constitutes a valid consent only if voluntarily given. This element of informed consent requires conditions free of coercion and undue influence.
Undue influence also includes offers of an excessive, unwarranted, inappropriate or improper reward or other overture in order to obtain compliance. Also, inducements that would ordinarily be acceptable may become undue influences if the subject is especially vulnerable as in the case of targeting children, persons with limited capacity, and elderly with elements of mental defect, or instilling fear.
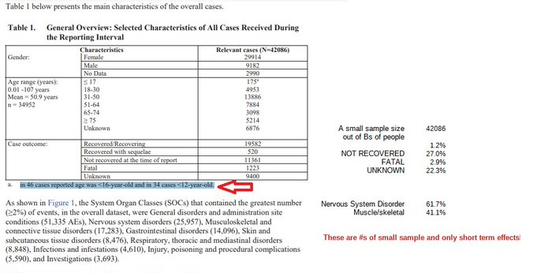
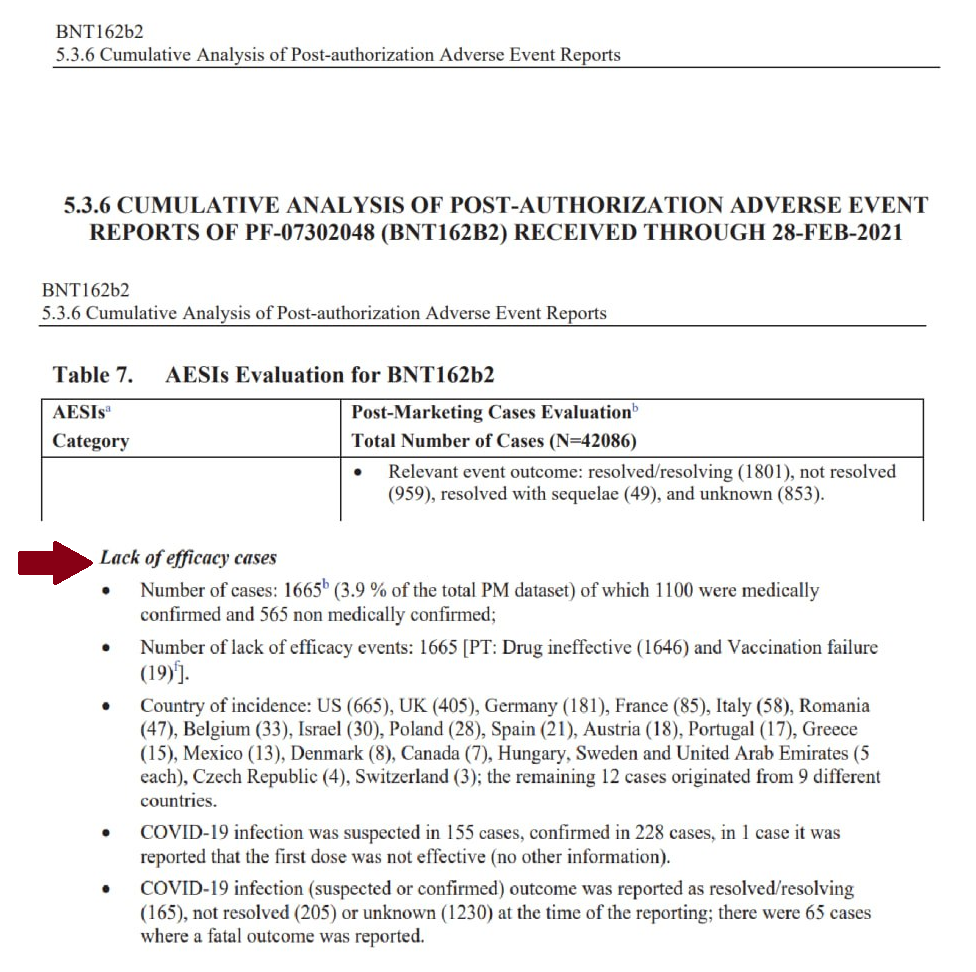
Short term morbidity and mortality cases from the shots are well reported and known, such as death, myocarditis along with spontaneous cardiac arrest with no warning, debilitating neurological conditions, etc. And, there is no means yet to determine mid and long term effects because Phase I trials have not been competed, let alone Phase II and III - which is vital information in order to determine informed consent.
Injustice has been performed with companies and government representatives, by involving vulnerable subjects, including the young, those unable to fully comprehend with all necessary information, and scaring parents with compromised capacity for free consent. In addition to lack of individual, tightly scheduled, continual monitoring and follow ups, autopsies of all persons involved in this trial participation should be conducted for reporting by the pharmaceuticals companies for any and all persons who received the shots, as well as labs determining efficacy and detriments (as examples, antigen creation, D-dimer, Pulse Cardiac and Troponin Tests) for all those who were coerced or unduly influenced to participate in research.
This law was created to protect people from government abuse through experimentation. The government cannot arbitrarily dismiss components, create resolutions or stipulations to supersede the law, as to invalidate its protection of individuals from them, including, but not limited to Health and Human Services (HHS) Center for Disease Control (CDC), Food and Drug Administration (FDA), National Institute for Health (NIH), etc. and pharmaceutical companies, etc.
Persons have been illegally acting as members of, or bypassing, IRB safety review and monitoring of each and every person receiving injections, with open undue influence and coercion, to participate in Covid injections. Coercion has been especially directed to the diminished autonomous, children and elderly, through TV ads, library recordings, verbal encouragement, schools or other public venues acting as government agents, and/or clinical researcher recruiting participants, and/or illegally as untrained IRB member who is not following up to ensure safety of the people they recruited, coerced or used undue influence.
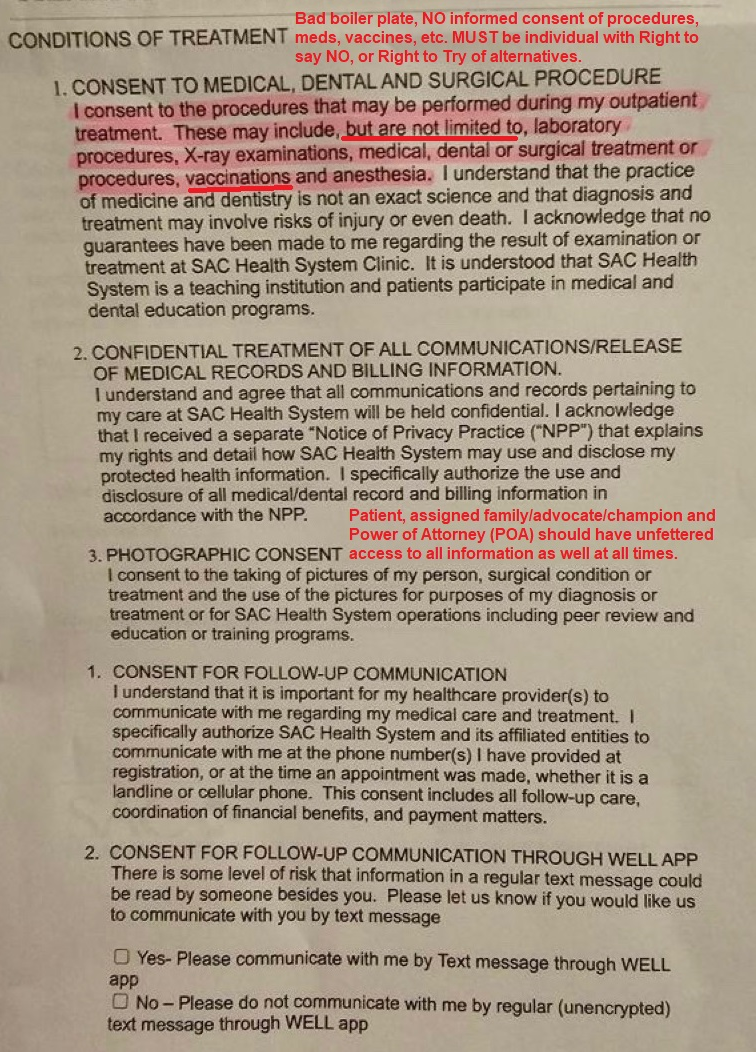
Overall lack of informed consent has become too often common practice across the healthcare industry, including people being given consent forms hours or minutes prior to surgery; no alternative treatments or lifestyle-nutrition changes prior to medications begin prescribed, and undue influence to intubate or perform surgery on patients in lieu of alternative treatments.
Dismantling PREP ACT pages 96-98 Kaiser, Newsom Court Case |
| ||||||
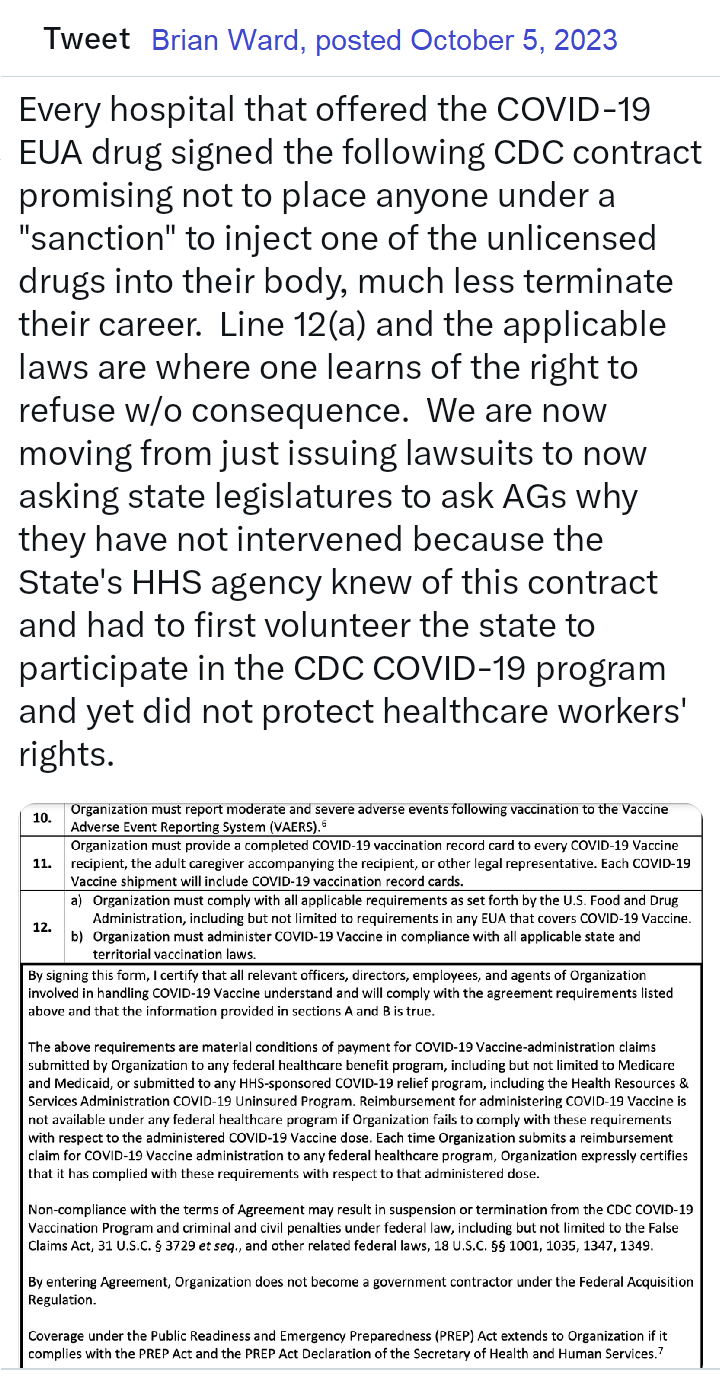
Lawsuits for unconstitutional violation of laws regarding shots
Guess what? Defendants in our lawsuits no longer argue that they had a right to mandate EUA drugs due to their state's at-will employment doctrine. That the EUA drugs can be mandated. That they had the authority to even issue the mandate. Why? Read the 127 pages, and then you'll understand that it was a legal lie from the beginning, but due to the novelty of the laws, no one knew of them. As courts have stated, "sometimes laws take naps," and these laws never showed up for work until now. https://coloradomedicalfreedom.com/wp-content/uploads/2023/08/Stamped-Final-Complaint.pdf
full document https://coloradomedicalfreedom.com/wp-content/uploads/2023/08/Stamped-Final-Complaint.pdf
page 127
C. the Secretary has no “authority to require any person to carry out any activity that becomes lawful pursuant to an authorization under this section…” 549. In 2005 Congress passed the PREP Act94 which provided the following regarding preemption of state law: (8) During the effective period of a declaration under subsection (b)…no State or political subdivision of a State may establish, enforce, or continue in effect with respect to a covered countermeasure any provision of law or legal requirement that— (A) is different from, or is in conflict with, any requirement applicable under this section; and (B) relates to the…administration…of the covered countermeasure, or to any matter included in a requirement applicable to the covered countermeasure under this section or any other provision of this chapter, or under the Federal Food, Drug, and Cosmetic Act [21 U.S.C. 301 et seq.]. 550. Therefore, via the PREP Act and 21 U.S.C. §360bbb-3, Congress expressly prohibits Defendants from: A. interfering with the authority of the Secretary, B. establishing a condition not authorized by the Secretary, C. establish conditions contrary to the Secretary and the congressional statute under 21 U.S.C. §360bbb-3, D. mandate participation in any 21 U.S.C. §360bbb-3 product or PREP Act activity, E. interfere with an individual considering participation in a 21 U.S.C. §360bbb-3 product or PREP Act activity, F. penalize a person refusing to participate in a PREP Act product or activity or 21 U.S.C. §360bbb-3 product. 551. The executive branch of the United States Government purchased all COVID-19 licensed and EUA drugs using federal funds. Congress expressly prohibits the federal government
Breaking…Gov Gavin Newsom and Kaiser have been sued in federal court for requiring healthcare workers to inject an experimental drug into their bodies as a condition to sell their labors in the marketplace. The requirement violated the workers’ Equal Protection of Laws and Due Process rights. Moreover, Kaiser signed a contract with the CDC promising not to mandate participation but did so anyway. Kaiser and Newsom fraudulently concealed the fact that nurses would be required to forfeit litigation rights if they incurred an injury from the use of the experimental drug. The California Nurses union stood by and refused to stop Newsom’s tyranny, leaving members without representation. Governor Newsom perpetuated the greatest assault on the US Constitution in the state’s history and the CA AG did nothing to prevent it. Worse yet, is that CA and Kaiser already had an agreement with HHS promising to never place an individual under a sanction for refusing to inject federally funded experimental drugs into the body.
Last edited10:55 AM · Nov 10, 2023
| Governor Inslee and PeaceHealth hospital sued for requiring nurses to inject experimental drugs into their bodies without their free will and voluntary consent. It's like a real-life episode of Jekyll and Hyde. Read the lawsuit here: https://coloradomedicalfreedom.com/wp-content/upl The National Council of State Boards of Nursing and the Ohio Board of Medicine are requiring students to hand over their private identifiable biometric scans as a condition to take the nursing test. Notice the deflection in the message. They present facts as if they are lawful, meant to place fear in the hearts of nurses. But, they never say it's a lawful requirement, only why do you not want to give your scan. One does not have to answer this question. | Dr. David Martin: under 21 Code of Federal Regulations § 50.23 and 24 – Exception from General Requirements, it is illegal to make anybody participate in an experimental program using coercion. |
Legal Fact: Any state that penalized citizens or denied unemployment benefits to an individual terminated for the sole reason of refusing to inject an unlicensed investigational drug into their body violated the individual's Fourteenth Amendment Equal Protection and Due Process rights. The U.S. Congress conferred legal authority onto an individual to either accept or refuse an EUA product. Both options were enacted by a valid act of Congress and must be equally protected. Moreover, the Supremacy Clause of the Constitution denied that state authority from interfering in the chosen option. The state established what courts call an Unconstitutional Condition. SCOTUS said: "But the power of the state in that respect is not unlimited; and one of the limitations is that it may not impose conditions which require the relinquishment of constitutional rights. If the state may compel the surrender of one constitutional right as a condition of its favor, it may, in like manner, compel a surrender of all. It is inconceivable that guaranties embedded in the Constitution of the United States may thus be manipulated out of existence." Governors and state agency directors violated their oath of office & the Constitution the moment they required COVID-19 EUA participation and or penalized an individual's federally protected option. They deprived citizens of their interest in liberty and property and, unfortunately for some, their very lives, all without due process. They did so by applying the law unequally demoting those who refused to that of a second-class citizen.
12:45 PM · Aug 29, 2023
BREAKING: LA Superior Court requiring LAPD to reinstate an officer terminated for refusing the vax mandate. Full back pay too! This is under a Writ of Mandamus, which is rare.
2:18 PM · Aug 21, 2023
Last edited9:28 PM · Aug 2, 2023
The VERY first EUA issued was in 2005 for the Anthrax investigational drug for service members and civilian employees of the DoD. The EUA stated: A. Individuals (service members and civilians) who refuse anthrax vaccination will not be punished. (Emphasis added) B. Refusal may not be grounds for any disciplinary action under the Uniform Code of Military Justice. C. Refusal may not be grounds for any adverse personnel action. Nor would either military or civilian personnel be considered non-deployable or processed for separation based on refusal of anthrax vaccination. D. There may be no penalty or loss of entitlement for refusing anthrax vaccination, E. This information shall read in the trifold brochure provided to potential vaccine recipients as follows: You may refuse anthrax vaccination under the EUA, and you will not be punished. No disciplinary action or adverse personnel action will be taken. You will not be processed for separation, and you will still be deployable. There will be no penalty or loss of entitlement for refusing anthrax vaccination. Nothing in law has changed to negate the authority of DoD members to refuse EUA COVID-19 drugs except the 6 civilian appointees engaged in willful misconduct against our Armed Forces.
11:51 PM · Sep 3, 2023
by Rose M. Rohloff
Providing informative snippets from 100,000s of primary source documents.
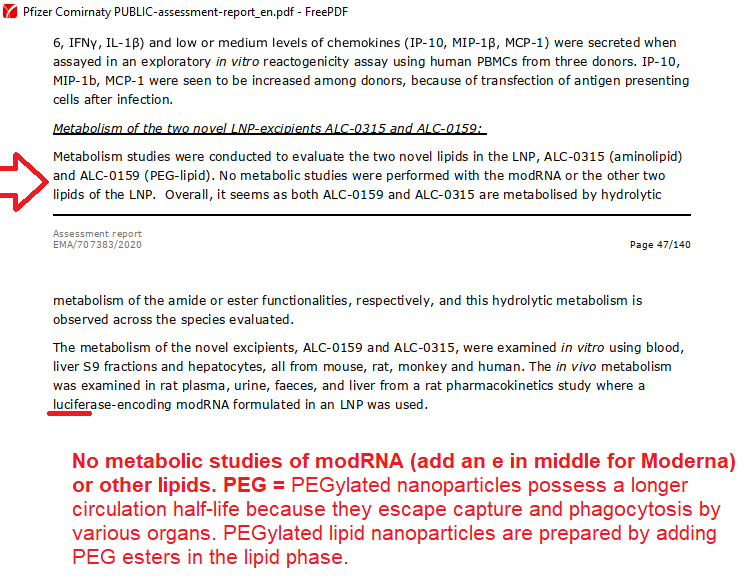
Chimera used for creation, efficacy testing (human+animal); Humanized mice from injected aborted fetus cells, to create LUCIFERase encoded modRNA: active substance is SPIKE PROTEIN.
Full Report to Department of Defense Inspector General (DoD IG) by Major Joe Murphy USMC Marine Program Liaison - former DARPA | |||||||
| darpa_jag_marine_letter_redacted.pdf | |
| File Size: | 7739 kb |
| File Type: | |
| PEG is a known carcinogen. Testing children in 2020 with deaths, released rpt April 2021
| |||||||
World Council For Health - Detox Protocol https://worldcouncilforhealth.org/resources/spike-protein-detox-guide/
| pfizer_comirnaty_public-assessment-report_en.pdf | |
| File Size: | 3929 kb |
| File Type: | |
| pfizer_5.3.6-postmarketing-experience.pdf | |
| File Size: | 1007 kb |
| File Type: | |
| pfizer_study_organ_sites_pharmacokinetics.pdf | |
| File Size: | 193 kb |
| File Type: | |
read blog entry 9/24/23
The 1974 National Research Act, what you should know & why Legal Cases around the country posted by Brian Ward
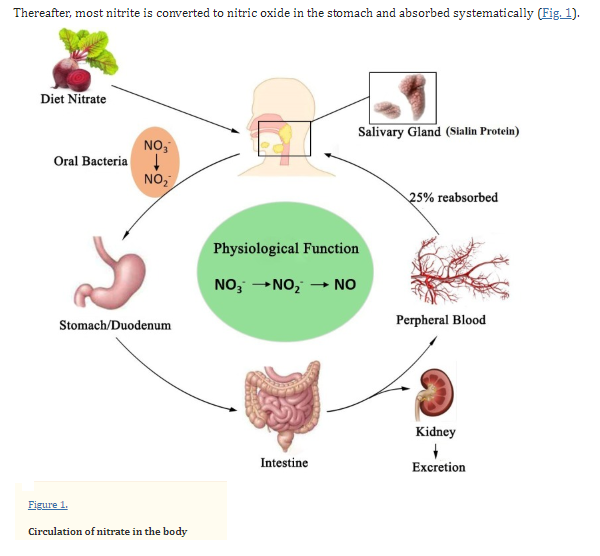
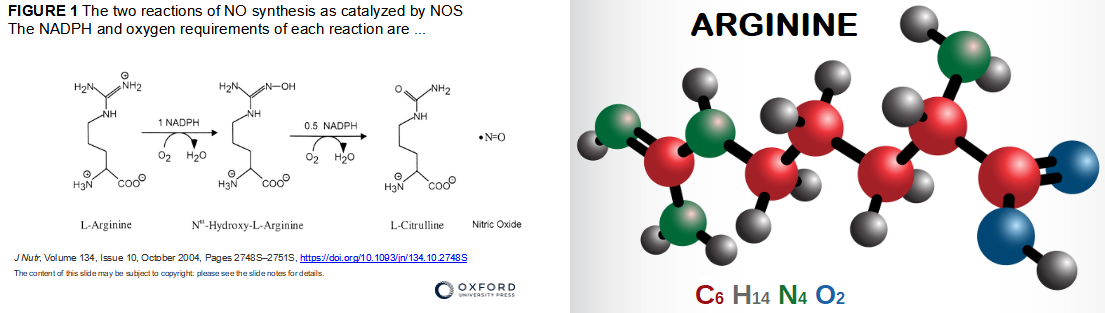
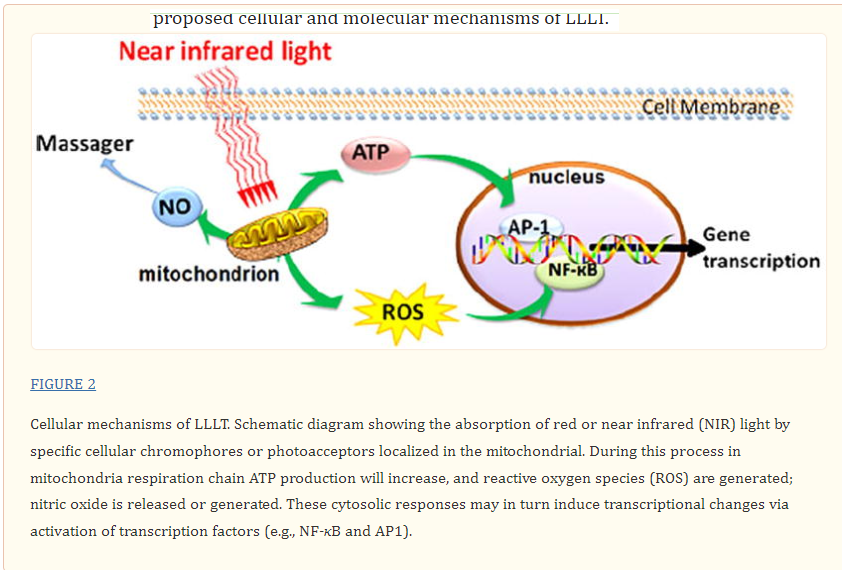
Nitric oxide (NO) - why you should know about this most important gas, created in our bodies
10/5/2023
by Rose Rohloff
Robert F. Furchgott, Louis J. Ignarro, and Ferid Murad shared the Noble Prize in 1998 for their discoveries concerning nitric oxide as a signaling molecule in the cardiovascular system
Sept 09, 2021
Giuseppe Fiorentino 1 Antonietta Coppola 1 Raffaele Izzo Anna Annunziata Mariano Bernardo Angela Lombardi Show all authors
"Strikingly, patients treated with L-arginine exhibited a significantly reduced in-hospital stay vs placebo, with a median (interquartile range 25th,75th percentile) of 46 days (45,46) in the placebo group vs 25 days (21,26) in the L-arginine group (p < 0.0001); these findings were also confirmed after adjusting for potential confounders including age, duration of symptoms, comorbidities, D-dimer, as well as antiviral and anticoagulant treatments." Read full Lancet article
- "Nitric oxide, having a free electron, is a free radical, making it an interesting signaling molecule. NO functions as a neurotransmitter, a macrophage-derived host-defense molecule, inhibits platelet aggregation and endothelium adhesion molecule expression, is an antioxidant, and is a potent vasodilator [1,2]. Nitric oxide is an endothelium-derived relaxing factor (EDRF)...Due to its many roles, loss of NO bioactivity contributes to disease in a variety of conditions including hemolytic anemias like sickle cell disease [8], transfusion of older blood [9], and endothelial dysfunction that occurs in pathological conditions like metabolic syndrome [10]" NIH article
- Affects major systems: platelets, ovaries, neuro, cardiac ... inflammatory response
- Issues with clotting, collagen, hypertension, fertility, etc. ....
| ... Deep dives into NO are needed for an individual's health - educate yourself, and then discuss with clinicians. | Nitric Oxide Signaling in Biology
| ||||||
Are we only beginning to understand this amazing gas, and the miraculous function of the body?
Protecting our families, especially children medically in the system - avoid medical kidnapping
5/27/2023
by Rose RohloffWrite something about yourself. No need to be fancy, just an overview. The current fulminated issues of "hospital kidnapping", and denying Rights of parents has existed for decades. Now health systems are using Department of Children Family Services (DCFS) to enforce. The following are true, documented cases of families, spanning decades, fighting hospitals for the health of their children. |
| Other parents, and children of elderly parents, across the country are experiencing similar situations of coercion, threats and intimidation from hospital administrators - including calling DCFS and the police; forcing families to hire expensive lawyers to even get a basic second opinion from a clinician they trust, and the stress with fear of actually having to go to court to fight for their loved one's Rights, who are being held (kidnapped) |
| One example of a form. A signed form should include the responsibility of hospital, staff enforcing quality care standards (e.g. to avoid hospital acquired infections and conditions), ensured care planning and care coordination, etc. Blanket consent is not informed consent, and should not include coercion upon ER visit with emotional compromised states. Being a signed form, a copy should always be immediately given to the person signing. |
| There are many classifications of drugs used for cardiac and vascular (CV) issues. A 2007 report is cited below, with his overviews by drug classification. The full article can be read with this link. |
Neuropsychiatric Consequences of Cardiovascular Medications
by Dr. Jeff C. Huffman
Associate Professor of Psychiatry at Harvard Medical School and the Director of the Cardiac Psychiatry Research Program in the Massachusetts General Hospital (MGH) Division of Psychiatry and Medicine.
Angiotensin-converting enzyme inhibitors
https://pharmaceutical-journal.com/article/news/from-snake-venom-to-ace-inhibitor-the-discovery-and-rise-of-captopril
Beta-adrenergic blocking agents or Beta (β)-Blockers
Calcium channel blockers (CCBs)
Diuretics
Doctors should always monitor electrolyte levels (sodium/Na and potassium/K+) of their patients taking diuretics.
Centrally acting agents - Antiadrenergic agent
Bottom line: Methyldopa is clearly associated with fatigue and sedation. In contrast to early studies linking methyldopa with depression, later reviews and studies have found this association to be relatively weak. Other neuropsychiatrie symptoms are uncommon.
Bottom line: Reserpine is associated with both sedation and daytime fatigue. Incidence of depression may be elevated among patients taking reserpine. However, other (generally more recent) reports question this association."
α-Adrenergic agents
Vasodialtors
Antiarrhythmic medications
Bottom line: Class III Amiodarone is associated with thyroid abnormalities in 15% of patients, and untreated thyroid dysregulation can lead to a variety of mood, cognitive, and psychotic symptoms. In contrast, direct neuropsychiatrie effects of amiodarone are uncommon.
Bottom line: Digoxin is associated with delirium and other cognitive effects, especially in toxicity. Visual changes and hallucinations may also occur with digoxin use, even at normal serum levels."
Conclusion by Author
Patients and their families know the cognitive baseline of individuals being prescribed medications, and therefore, should always monitor for any neuropsych impact seen if CV drugs are used, on an individual basis for what is safe per person. Any and all side effects should be know, along with contradictions to other drugs, for all medication being taken.
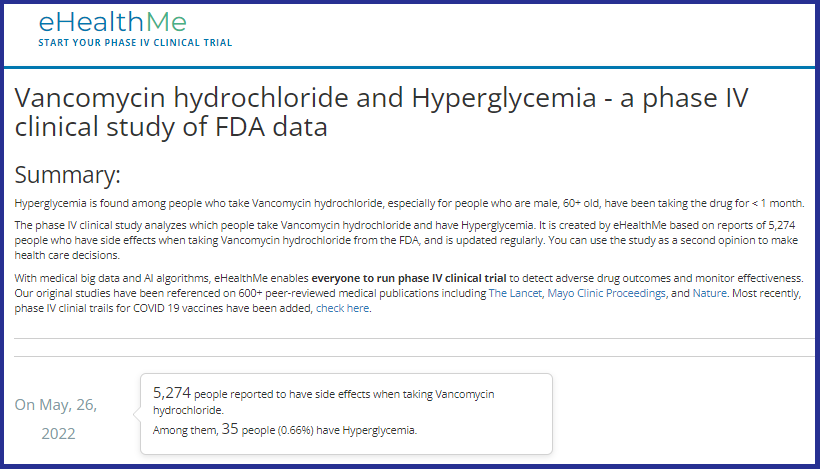
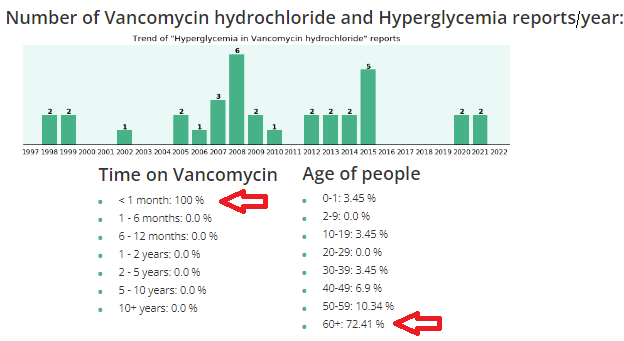
What should you be aware of regarding Vancomycin?
| Vancomycin (Vanco) is an antibiotic, in the classification of Glycopeptide used for gram (+) bacteria, typically used for: Methicillin Resistant Staphylococcus Aureus (MRSA); Clostridium Difficile (commonly called C-diff), a potentially deadly infectious |
Clinicians (nurses, doctors, physician assistants, etc.) are supposed to do comprehensive history and physicals (H&Ps) before using any drugs or treatments. And, it is important to know underlying conditions before using Vanco, because it can raise glucose levels, especially in diabetics, and/or cause kidney (renal) insufficiency, especially in elderly.
"I don't know what the average "lay person" does when they don't have all this information, and without a medical person to look out for them."
"This article is exactly why they stopped Vanco when he had his MRSA infection. His kidneys were starting to get compromised, so they immediately stopped it and started him on a different antibiotic, Daptomycin, which worked just as well and had less side effects for his kidneys and diabetes. Thankfully they caught it very early because of the blood tests they were doing to see what was happening. The new antibiotic was infused only once a day as opposed to twice a day Vanco, and there weren't all the extra blood draws to make sure the kidneys and glucose were doing okay. God is really in control and watching out for us, because the medical field doesn't always do that, even with a fellow medical person."
Vanco and high glucose/hyperglycemia
Vanco and kidney (renal) failure
Abstract A progressive increase in vancomycin resistance with consequent treatment failure has been observed in staphylococci. Therefore, new dosing guidelines advocating much higher vancomycin doses have been issued. Target trough levels of 15-20 microg/ml are proposed. Whether and how these targets can be achieved in patients with chronic kidney disease or those on dialysis are still under evaluation. The higher vancomycin doses to achieve these treatment targets carry a substantial risk for nephrotoxicity. This risk is incremental with higher trough levels and longer duration of vancomycin use. Critically ill patients, patients receiving concomitant nephrotoxic agents, and patients with already compromised renal function are particularly at risk for vancomycin-induced nephrotoxicity.
Acute kidney injury during daptomycin versus vancomycin treatment in cardiovascular critically ill
An India folklore, regarding lack of awareness, demonstrates the current myopic view of various specialists, who look at isolated symptoms without comprehensive assessments, resulting in poor or lack of diagnosing of real issues to address in patients. The industry push to eliminate primary care, teaching people they don’t need a primary doctor, or using primary care doctors as simple pass-through without diagnosing, handing off to multiple other doctors, has resulted in the loss of care coordination, overdosing multiple medications with contraindications/side effects, with increased conditions because multiple doctors only look at their individual view.
Long ago, old blind men were curious about the many stories they heard about elephants. The men were led to one for each person to independently touch the animal.
- The first blind man reached out and touched its side. "An elephant is smooth and solid like a wall!" he declared. "It must be very powerful."
- The second blind man put his hand on the elephant's limber trunk. "An elephant is like a giant snake," he announced.
- The third blind man felt the elephant's pointed tusk. "I was right," he decided. "This creature is as sharp and deadly as a spear."
- The fourth blind man touched the elephant's leg. "What we have here," he said, "is an extremely large cow."
- The fifth blind man felt one of its giant ears. "I believe an elephant is like a huge fan or maybe a magic carpet that can fly over mountains and treetops," he said.
- The sixth blind man gave a tug on the elephant's coarse tail. "Why, this is nothing more than a piece of old rope." he scoffed.
| The six blind men determined what they knew on limited assessment of only touching one part of the elephant, just as individual doctors only look at single symptoms; for example, cardiologist only looks at the heart, nephrologist only looks at kidney, endocrinologist only looks at the endocrine system ... |
Calm intelligence, professionalism, logic and sense. Nine (9) doctors interviewed https://www.bitchute.com/video/2JPy7qZiXvNr/ regarding Covid, Hydroxychloroquine (HCQ) and masks.
| The mother called the Urgent Care center and they informed her she got bad information, they would absolutely not do a swab from the car, she must come in. She stated, “You want me to walk into that center with sick people along with my two other smaller, healthy children so in less than a minute you can swab my other daughter’s throat to verify if she needs an antibiotic?” They told the mother that she could not bring that many people into the facility with her. The mother asked, “What exactly to do you expect me to do then to protect myself, and what do you want me to do with my other kids?” The healthcare personnel demonstrated panic, without some basic sense. I finally asked the mother what she wanted to do. She stated, “My daughter is alert, drinking, not that bad. I am going to get Zinc and good foods, push fluids especially with warm lemon and honey, have her gargle with warm salt water, and see how she is in 24 hours.” The daughter’s temperature was 99 by nightfall, and 98 degrees by the next day without a sore throat. If the mother had not questioned the panic of the doctor and nurse, her daughter would have been put on an unnecessary antibiotic, opening her up to secondary infections, and exposing herself to unnecessary virus and bacteria while being immunosuppressed. | From the NIH Amoxicillian: Additionally, there is a moderately increased risk of secondary Clostridium difficile (C-diff) colitis when compared with other classes of antibiotics. Females taking this medication can also develop vaginitis secondary to vaginal mycosis or candidiasis. (Our bodies keep C-diff and candidiasis in check with our needed good bacteria.) The next day, the mother stated, "The doctor lost all credibility with me going on in a panic about the issues with the COVID-19, "this will never end by Easter, etc." when the hospitals have little volume, no reported cases. "She refused to do any history and basic assessment to swab my daughter to rule out strep before writing a prescription." Our healthcare system has been broken regarding the lack of some basic sense at the ground level, with reactionary versus proactive care; missing great primary care doctors, avoiding the quick symptom = writing a prescription form of care. |
- Great education nationally in diet to strengthen the immune system. Great nutrition understanding regarding what vitamins to focus on, removal of sugars from the diet, etc. The idea of waiting on vaccines after the fact, for every virus, is not realistic or proactive.
- Better testing of high risk patients regarding their health with focus on strengthening their own immune system.
- Zinc and other nutrients when one is immediately feeling poor. Fights inflammation, works with immune system or exposure to infectious persons.
| Health Rosetta hosted a wonderful webinar with Chief Medical Officers (CMOs) from around the country speaking, without panic, about the effective care of their patients at home with COVID-19. Their stories demonstrating the importance of shifting back to great primary care. |
Hopefully, many good things will come from this virus experience to positively shake up our healthcare system, including basic sense procedures, with the importance to rebuild and focus on great primary care again. Another glaring issue to address is the role of clinicians as cool, calm professionals, removing emotion when instructing with full information, with clearly explained options for informed consent and decision-making for delivery of quality care.
by Rose Rohloff
Championing care: knowing your individual baselines, understanding trending deviations, influencing factors.
| A Wall Street Journal (WSJ) article https://lnkd.in/e9awgQT 1/24/2020 posted wrote: "Nearly 150 years ago, a German physician analyzed a million temperatures from 25,000 patients and concluded that normal human body temperature is 98.6 degrees Fahrenheit. That standard has been published in numerous medical texts and helped generations of parents judge the gravity of a child’s illness. But at least two dozen modern studies have concluded the number is too high. Or was it? In a new study, researchers from Stanford University argue that Wunderlich’s number was correct at the time but is no longer accurate because the human body has changed. Today, they say, the average normal human-body temperature is closer to 97.5 degrees Fahrenheit." | Championing your own health is about understanding your healthy baselines. Just as individuals have a variable "healthy" baseline for their blood pressure and heart rate, why would an individual not have an individualized, normal baseline for their temperature? And, temperatures are now measured using different methods: forehead-ear-mouth-rectal, producing deviations based upon how the temperature is obtained. It is important to understand, compare what mechanism was used to take the temperature. Is your normal 98 degrees, while another may run 97 degrees? Is the person normally running 97 degrees now have a temp of 99 along with malaise, dehydration because they are fighting a virus or bacteria? Assessment/vital sign numbers provide more information for clinicians (Doctor, PA, Nurse, etc.) when provided in context of associations, trends, baselines and influencing factors. |
It is known taking medications will impact various lab values. For example, Diuretics e.g. Lasix (Furosemide), can cause low potassium levels. There is an interesting article in Medscape, Which Drugs Interact With Lab Tests? Jun 18, 2019., addressing the fact that certain medications can also interact with the actual processing of certain lab tests causing inaccurate results.
A recent view of the prescribing information for 1368 prescription drugs found that 134 (9.8%) included information about a specific lab test interaction, 31 (2.3%) stated that the drug did not interfere with lab tests, and four stated that there was no available information.[1] ... | Patients, families and caregivers need to be aware of what name, class, internal action, as well as all other medication interactions for every medication, vitamin and supplements being taken. As Dr. Scott shares as insightful, it is also important before getting lab values done to understand if any medications being taken will impact labs to be processed and cause false results. |
by Linda Lybert
President/ Healthcare Surfaces Expert, Founder/Executive Director Healthcare Surfaces Institute
A 40-year old mother went to the doctor after treating herself holistically for some laryngitis, stuffy nose, congested sinus, with continued symptoms after five days. After an exam, the doctor stated, “I am not going to give you antibiotics. You do not have a fever; your lungs sound clear. It looks like a little virus with severe allergies. I recommend an antihistamine.” The patient told him, “Thank you for not putting me on antibiotics when they are not needed, that makes me happy.” He responded, “I am glad you are glad.”
This story is sadly too often the new normal, numerous instances of patients and their caregivers stating issues of diagnosing with medication prescription, or misdiagnosis; the doctor or nurse having no idea of pre-existing conditions or a full list of medications currently being taken, a lack of care coordination or care planning because the time was not taken to simply read the chart (whether written or electronic), and ensuring a comprehensive history followed by the necessary physical assessment.
No physician or nurse should walk in to care for a patient without first having read the patient’s record, knowing all current information, the last visit/healthcare encounter, chronic conditions/comorbidities, and all medications; then, asking for updates of changes. Unfortunately, even without having to decipher poor handwriting, being able to read clean typed text, clinicians are not simply reading the basics of information they should before doing any diagnosis, planning and care, or prescribing of medications.
by Rose Rohloff
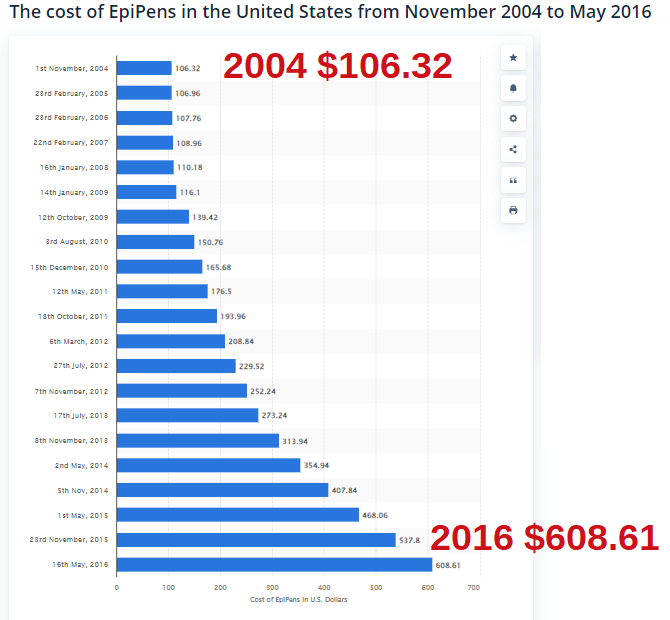
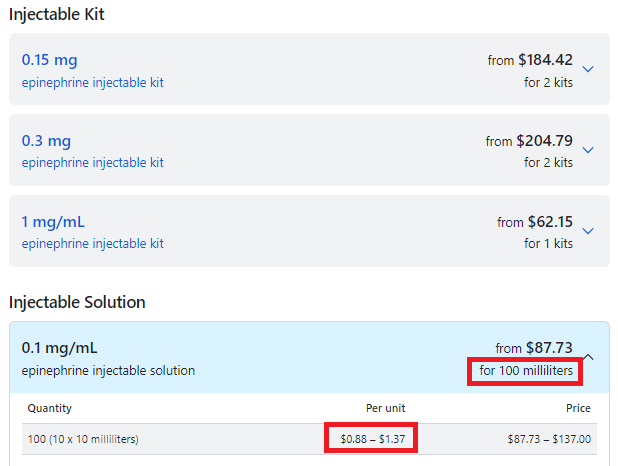
| This needs to be addressed at the State & Federal levels - fighting the unconstitutional Federal violation of the Sherman Antitrust Act of 1890 by Congress and the Executive Branch. [The Federal Gov is also violating pushing for Narcan to be in every household - pouring gasoline on fires - because now people think they can be saved continuing to overdose on street drugs, especially Fentanyl: read NARC PARTY - OPIOID CRISIS AND SURGEON GENERAL ADVISORY | How Mylan, the maker of EpiPen, became a virtual monopoly - The Washington Post washingtonpost.com› business › economy › 2016 › 08 › 25 › 7f83728a-6aee-11e6-ba32-5a4bf5aad4fa_story.html August 26, 2016 - The company lobbied lawmakers — both directly and indirectly — to increase the availability of epinephrine autoinjectors in U.S. schools. |
Use Case: A police officer was having hives and went to an emergency room. The staff asked him if he wanted an EpiPen. His response, "What the hell is it? The staff did not educated him, provide one to him to use if he felt he needed it. I informed him to read the fine print = it was a dose for a child an not a grown 200lb man, with an expiring date in a couple of weeks.
| On November 13, 2013, President Obama signed into law the School Access to Emergency Epinephrine Act. The federal legislation provides a financial incentive for states to enact their own laws requiring schools to keep non-student specific epinephrine auto-injectors in case of an emergency. And so, the Federal Government created an illegal monopoly for company who owns the patented auto-injector, not the medication, followed by price gouging, especially for times of crisis, and finally panicked outrage in the public. |
|
| 'There's nothing to give them': Patients, pharmacists scrounging for EpiPens Full story Patients and pharmacists nationwide are grappling with a persistent shortage of Mylan's EpiPen, forcing some to travel great distances or go through several hoops to access the lifesaving allergy treatment, according to Bloomberg. EpiPens have been difficult to obtain since at least May 2018, when the FDA alerted the public to the shortage. |
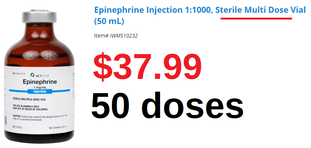
| Cheaper "do-it-yourself" alternative EpiPen may carry more ...https://www.cbsnews.com/news/cheaper-epipen-alternative-may-carry-risks/ The cost is about $20 - $15 for a syringe and $5 for a vial or two of the drug. |
Summary
- Obama signed into law an illegal monopoly
- The Mylan company does not control the patent on the drug epinephrine, only their autoinjector Epipen.
- Epinephrine comes in multi-does vials: EpiPens are only single dose!
- CDC stats read 4%-6% have food allergies, only .001 of the population has anaphylaxis to nuts + shell fish, the biggest allergy issues, 63 to 99 deaths occur each year in the United States due to anaphylaxis.
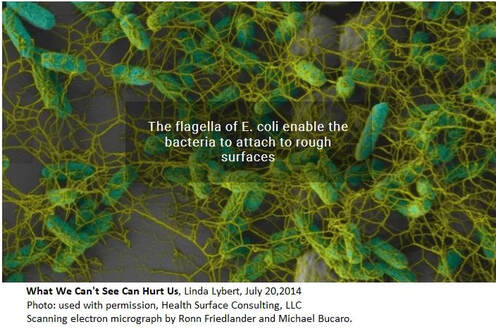
A popular trend in houses is the use of marble and granite as counter tops. A leading surface expert, Linda Lybert President of Healthcare Surface Consulting stated, “Granite and Marble are like large sponges you cannot wring out.” The photo displayed shows the build up of E. coli bacteria in the pores of stone. According to Ms. Lybert, even when sealed, the porousness is reduced, but not eliminated. And, bleach is not able to eliminate once they reside in the crevices.
As the elderly begin to lose their mobility and agility, it is important to maintain clean surfaces in bathrooms and bedrooms, along with the most important surface being the skin. Diligent hand washing and bathing is important throughout the day to avoid cross contamination from the loved one you are caring for, as well as to them. The other surface area to be conscientious of is bedding. When excrement accidents occur, it is important to wash bedding with very hot water to not only clean them, but also kill the microbes.
Clostridium difficile (commonly known as C-diff) "is in the community and found in outpatient settings. There are significant risk factors in patients who are immunosuppressant, individuals who have been on antibiotic therapy, and the elderly population." C-diff is a secondary, very dangerous and potentially deadly infection after antibiotic use. [read article] It is important to those in the community to have appropriate antibiotic prescriptions and use, especially avoiding unnecessary broad spectrum antibiotic use which targets the "good" bacteria you need internally (and not on external surfaces) to kill off C-diff.
by Rose Rohloff
But, what is value? Is society conditioned to accept low quality as value, because a lower standard has become the norm?
| Value is a relative term based upon personal perception, and oftentimes great marketing. True value is based upon insightful knowledge of what entails quality along with the cost of delivering goods and services. Value-based care is the new buzz for basing reimbursement in the healthcare industry. But again, what is value care: personal perception, marketing, cost? |
The primary issue with such score deviations is determining if poor marks are isolated instances (one offs); or, if the variance of only highest and lowest reflect the knowledge of reviewers. Are the high ratings from non-healthcare persons based on perception of the veneer friendliness and scheduling, with one star comments based on specific quality requirements, care competency posted by those with healthcare insight/experience?
As a 35+ year healthcare veteran, an answer was determined accompanying a Medicare patient ‘John’, in his mid-80s who experiences early stage dementia, to the office for a post-op visit for a leg stint placement.
| Upon arriving, another elderly patient (80s) was sitting outside, unattended in wheelchair, hot sun, 100 degree weather, no water. When asked why he was there, he stated, “I can’t stand the freezing air conditioning inside while waiting for a ride.” After walking John into the lobby, the gentlemen clearly seen through the glass door was pointed out to the receptionist stating that he was left in hot sun, no water, unattended. The receptionist stated, “It is his choice to stay out there.” I then stated, “Get someone to check on him, give him water, put him in the shade and check when his ride is supposed to arrive and monitor him if it is delayed or bring him inside.” One person escorted us back to exam room. She did not introduce herself or her title. She proceeded to take the blood pressure with no other vital signs (unknown if a secretary, an aide, a nurse or tech). She then asked the patient, “How much do you weigh?” He gave a number. As patient champion I responded, “He doesn’t know, he has not weighed himself. You need to weigh him yourself.” She responded, “We don’t have a scale.” She then left. I followed her witnessing her documenting the incorrect data. | I reiterated he has dementia with no idea how much he weighs. She replied, “It doesn’t matter anyways, we just need to put something in the record.” She was reflecting an 11 pound weight loss from previous recording. It is unclear if they performed the previous weighing, if it was done just prior to surgery to determine proper anesthesia delivery for his surgery. Another woman in scrubs entered the exam room without introducing herself or her title, asking John to remove his shoes and socks. (The scheduled appointment was with the PA so the patient assumed her identity.) She asked him if his wound was healed and he replied, “Yes.” She documented something in the chart without ever assessing his wound for healing or determining if there was infection. She bent down and felt his feet with her whole hands stating they feel warm, and then asked if he had numbness in his feet. John responded, “Yes.” | Having worked as a registered nurse (RN) in cardiovascular and neuro intensive care units (ICUs), I know she never did pedal (foot) pulse checks x4 comparing both feet. She never assessed location of numbness, or if chronic/intermittent, positional with sitting/, standing, walking, etc. The family had asked if aspirin could be stopped as the patient has experienced nose bleeds in the past. The staff person responded yes and since there was 90% blockage of the previous stint, it was cleaned out and continue Plavix. There was no establishment of lab work as part of care plan determining effectiveness of the medications, especially since the previous stint occluded. "1,750 or so stent patients are also prescribed Plavix to prevent clots from forming around the stent, but of that group, approximately 500 (29%) carry a genetic variation that prevents them from converting Plavix into its active form. This gene-related lack of response stands to be "especially severe" in about 50 (3%) of those patients, who won't derive any benefit from Plavix - 2010 Vanderbilt Medical Center |
Perceived value based on quality versus true value and cost
The care competency and quality as true value-based care during the visit includes:
- lack of basic cleanliness standards with severe cross contamination practices
- no introduction of name or title of any staff member
- fraudulent documentation in the electronic medical record (EMR)
- no assessment performed during a specific post operative visit (a family member could have taken the BP and said his feet felt warm.)
- lack of care planning and evaluation of medication regime
- unnecessary secondary office visit charging for follow up
- another elderly patient left unattended in the hot sun
If the U.S. healthcare system wants to achieve true value-based care, we need an educated population, higher accountability of staff standards with the ability to send evaluations direct to payers based on specific facts and not emotion, and surveys must include care competency reviews versus only veneer questions of politeness, room appearances, and on time scheduling.
click an article
to read and post comments
Search topic
select category
All
APAC Teams
Care Quality
Champion Your Own Care
Clinician Quality Education
Experience Satisfaction
Healthcare Consumerism
Health Innovation
Medical Care Coordination
Palliative Care
Patient Engagement
Physicians
Population Health
Transitioning Care Coverage
search by date
July 2024
June 2024
April 2024
March 2024
February 2024
January 2024
November 2023
October 2023
June 2023
May 2023
October 2022
September 2022
July 2022
August 2020
April 2020
January 2020
June 2019
May 2019
April 2019
October 2018
September 2018
August 2018
July 2018
May 2018
April 2018
March 2018
February 2018
January 2018
December 2017
September 2017
June 2017
October 2016
September 2016
May 2016
March 2016
October 2015
June 2015